Health Strategy.
Dietary risk factors for cancer. An enormous body of research has been devoted to studying the relationship between dietary factors and breast cancer * * * * *. The reason for the special attention is easy to understand: diet is the most influential and most easily modifiable factor in our health *. It is estimated that nearly a third of all cancers can be avoided with the right diet and supplements * *.
But it's not just about cancer; nutrition is the cause and engine of many human diseases. Therefore, we can safely say that diet therapy is not aimed at treating any one organ or getting rid of any one disease. It aims to improve the whole body.
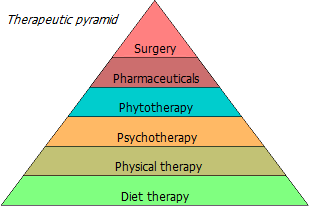
In accordance with the concept of the «therapeutic pyramid», any treatment should begin with a diet. If dietary modification, muscle loading, stress management and positive thinking, taken together, do not give a positive effect, one has to resort to more and more powerful methods – herbal medicine, chemotherapy and, finally, surgery.
In severe cases, it is necessary to start with the strongest treatment method, although the preparation of the treatment protocol is always left to the specialist. But in any case, lifestyle remains a fundamental factor in treatment. Including the diet, which can be not only a slow poison, but also a delicate medicine.
If the diet is not correct, then the rest of the treatment may be ineffective. On the other hand, there are cases when only one change in the diet led to the healing of many chronic diseases within a fairly short period of time, sometimes in 3-6 months.
The genes we inherit contribute minimally to the risk of developing cancer. The decisive contribution is made by lifestyle. The way we live, what we eat, what we drink, what we breathe and what we come into contact with. Food and drink entering the body can contain both directly carcinogenic substances (viruses, toxins, xenoestrogens) and substances that promote cancer indirectly. For example, causing insulin resistance (simple sugars), inflammation (meat, glycation products, many fats), proliferation (milk), and angiogenesis.
Breast cancer is a diet-sensitive tumor *. Food preferences affect the risk of cancer, starting from the earliest stage of development of the organism * * *. The female breast is especially vulnerable in adolescence, when it undergoes an accelerated proliferation of hormone-sensitive cells, which finally complete their maturation only during the last trimester of the first pregnancy.
Thus, a high consumption of animal fats during puberty in girls contributes to the development of a tumor in a later period of life * * *. The difference in pre-menopausal breast cancer risk between the group with the highest red meat consumption and the group with the lowest can be as much as 43% *. Just one serving of red meat during adolescence is associated with a 22% increased risk of premenopausal breast cancer, while the same intake of red meat in adulthood is associated with only a 13% increased risk *.
In contrast, if teens consume a lot of foods containing carotenoids (pumpkin, carrots, sweet potatoes, zucchini), nuts, beans, vegetable oils, vitamin E and fiber, and at the same time consume little animal fat, red meat and alcohol, then this may reduce their risk of benign * * and ER-malignant * breast tumors later in life. Replacing one serving of red meat with one serving of fish, legumes and nuts in the diet of adolescent girls is associated with a 23% lower risk of breast cancer in premenopausal women and 15% overall *.
As will be discussed below in numerous facts, modifiable risk factors play a central role not only in the occurrence of diseases, but can also decisively influence the elimination of them. In addition, dietary changes may improve the outcome of primary treatment. A case has even been described where, after a single change in diet, far-advanced breast cancer was reversed *.
Sure, the best diet is the one that is most adequate to the biology of the body. What kind of diet best suits human biology?
Adequacy of food to body
It is still not known for certain how quickly an organism can fully adapt genetically in response to changing external conditions. However, it can be assumed that the radical changes in lifestyle and nutrition that began during the times of the agricultural revolution and animal husbandry (about 10'000 years ago) happened in evolutionary terms too recently for the human genome to adequately adapt the anatomy and human physiology.
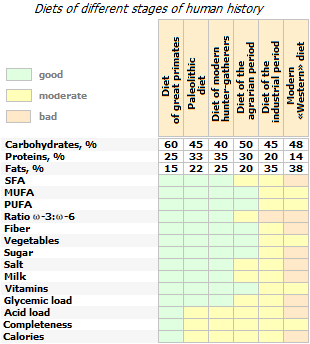
The modification of the diet during this time has seriously changed seven of its most important characteristics *:
1) glycemic load,
2) the amount and composition of fatty acids,
3) macronutrient balance,
4) micronutrient density,
5) acid-base balance,
6) sodium-potassium balance,
7) the amount of fiber.
The diet of modern man, in comparison with the diet of hunter-gatherers, is significantly depleted in trace elements and alkaline elements, such as potassium and magnesium, and the amount of fiber consumed has decreased by up to 10 times *. At the same time, it is enriched with saturated fats, simple sugars, sodium and chlorine *. The ratio of vegetable:animal food in the diet of a Paleolithic man was from 1:1 to 2:1 (depending on natural conditions and geographical latitude); while in the diet of a modern person this ratio is reversed *.
The resulting discrepancy between genetically determined biology and the style of nutrition, culture and activity of modern man is the cause of the growth of degenerative diseases. In order to become a healthy biological species again, a reasonable person should bring his diet in line with the program genetically embedded in him. If you can not adapt your body to modern food, it remains to adapt food to your body.
It is characteristic that in the wild, adult primates practically do not suffer from degenerative diseases inherent in humans, and even in old age they maintain satisfactory health. However, even small changes in their diet associated with captivity lead to a significant deterioration in their health and reduced life expectancy.
The addition of modern «human food», rich in fat and protein, causes «human diseases» in primates *. However, the mere existence of «human diseases» in humans suggests that modern human nutrition is just as inconsistent with human biology as it is with the biology of other animals. And that it's not really «true» human food.
It is significant to compare the health status of representatives of the same tribe of Papua New Guinea. Living in the wild, modern hunter-gatherers have a blood pressure of 105/65; their insulin response to glucose is 40% lower than that of Europeans; and body mass index – a quarter below (~ 20) *. At the same time, their fellow tribesmen, who changed their living conditions and diet to urban ones, have higher blood pressure and overweight, and significantly higher average levels of total plasma cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL), glucose fasting blood and glycated hemoglobin (HbA1c) *.
The largest study on risk factors for diseases (GBDS), has come to a convincing conclusion that the main cause of premature disability and death in the United States is the standard American diet. The top four types of foods that reduce the overall risk of death were those that have accompanied humans for many millennia – vegetables, fruits, nuts/seeds and whole grains *. The risk of breast cancer in this study steadily increased as the proportion of animal fats in the diet increased from 6% to 24%.
The author's study of dietary habits around the world revealed distinct differences in diet in countries with the highest and lowest incidence of breast cancer *. The most significant risk factors were the ratios of dietary fat to fiber and, in general, fat to carbohydrates. Proponents of various fad diets can justify their benefits in any way they want, but the facts stubbornly prove that the most healthy diet for a person is the diet of distant ancestors – rich in fiber and poor in dietary fat *.
The history of nutrition
First of all, let us turn to the diet of such higher primates as gorillas. There are several subspecies of gorillas, however the diet of the various subspecies seems to vary more from season to season than from subspecies to subspecies *. For example, compared to mountain gorillas (Gorilla beringei), the main diet of western gorillas (Gorilla gorilla) contains three times more fruits (43%) and leaves (12%) and less grasses (39%) *. However, the structure of macronutrients between these subspecies does not show a significant scatter. Approximately 79-97% of the diet of female gorillas is of plant origin, with the remaining 3-21% being insects, snails and larvae * *.
Gorillas devote most of their time to food because their food is low in calories. Adult female gorillas in the wild consume an average of 12 kg of plant foods, which is about 8 kg in human equivalent – three times the weight of food normally consumed by humans *. A vegetable diet provides female gorillas with at least 4'000 kcal/day of energy *, i.e. 2'700 kcal/day human equivalent.
The main part of the dry part of the gorilla diet is fiber – cellulose, lignans and other indigestible complex carbohydrates. All primates lack the digestive enzymes that break down fiber, so its energy is diverted to gut bacteria, which metabolize the fiber to form short-chain fatty acids (SCFAs).
The macronutrient profile of the gorilla diet is as follows: dietary fats up to 5.9%, proteins up to 57%, available carbohydrates up to 37.1%. In addition, a significant part of their daily energy requirement is provided by SCFA energy obtained from the intestinal microflora *. The ratio of saturated fatty acids to monounsaturated and polyunsaturated fatty acids from food is 3.2:1.3:5.5, and the ratio of fatty acids ω-6:ω3 is 1.44 *. Another source reports that dietary fat provides about 14% of the total calorie intake of gorillas, which is half that of the modern human diet.
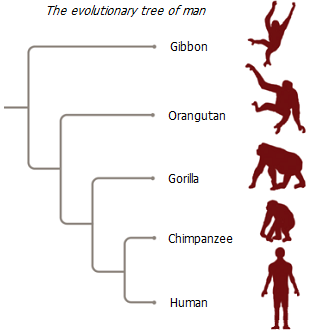
Gorillas are probably not the best object to compare with humans. These are practically pure vegans, and from the point of view of genetics, they are further away from humans than chimpanzees, which are genetically the closest biological species to humans. Chimpanzee DNA matches 98.4% of human DNA. Therefore, it would be more correct to turn to the diet of chimpanzees (Pan troglodytes). As with gorillas, cancer in wild chimpanzees is extremely rare, and so far no cases of breast cancer have been reported in female chimpanzees.
The diet of modern chimpanzees is ~ 75% ripe fruit and ~ 20% leaves and heartwood pulp, which, trees, mainly produce energy in the form of carbohydrates and proteins *. The average fiber intake is about one third of the total dry weight of food, which is exactly the same as fruit pulp. The amount of fat in the chimpanzee diet is very low (0.5-19%E) *.
Chimpanzee families use termites and reptiles as a source of protein. They also occasionally prey on smaller primates, however the average animal protein intake of adult wild chimpanzees is ~ 5% of total dietary energy (%E) * *. Animal protein is distributed extremely unevenly: it is eaten mainly by males who participated in the hunt. When chimpanzees are able to make conscious food choices, they maintain their total protein intake at ~ 12%E *. Some sources report the following energy ratio of carbohydrates:protein:fat in the diet of wild chimpanzees: 73:21:6 *.
In the most favorable case, the energy absorbed with food provides adult chimpanzees with a carbohydrate:protein:fat percentage of approximately 63:14:22. Or otherwise, daily ~ 50 g of fat, 70 g of protein and 320 g of digestible carbohydrates, including digestible fiber *. The daily calorie content is 2'000 kcal/day, i.e. 2'250 kcal/day in human equivalent. The ratio of digestible to indigestible carbohydrates is 1:2.4.
Other sources report similar dietary patterns for female chimpanzees: fat 6% dry weight, protein 13%, soluble carbohydrates (such as glucose, fructose) 13%, insoluble carbohydrates (such as starch) 43%, neutral fiber (such as lignin, cellulose) – 25% * *. The mass of food in terms of dry weight is 800 g, and its daily calorie content is 2'500 kcal. Almost the same as in the previous case, the energy ratio of carbohydrates:protein:fat is 63:16:21, and the ratio of digestible to indigestible carbohydrates is 1:2.3.
The chimpanzee gut microbiota is able to partially digest neutral fiber * *: ~ 50% of fiber is converted to short chain fatty acids (SCFA) with an energy yield that is thought to be comparable to that provided by water soluble carbohydrates. In other words, chimpanzees get about the same amount of calories from simple fats produced by gut bacteria inside the body as they get from water-soluble carbohydrates from outside. This important observation will be useful to us later.
The evolution from ape to man was accompanied by parallel anatomical and dietary changes. The first step was the transition to omnivorous. Already about 2.5 million years ago, early hominids (Homo habilis) increased the amount of animal products in their diet. This happened simultaneously with the development of bipedality, the discovery of stone tool technology, the modification of the dentoalveolar system, and the increase in brain size. However, a radical change in diet occurred about 1.8 million years ago, when Homo erectus appeared, whose habitat, under the influence of climate change, changed from fertile rainforests to less favorable savannah.
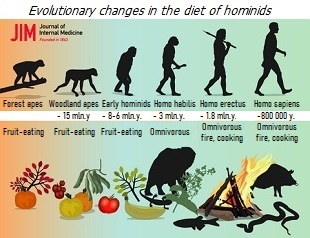
Due to global cooling, the fruits, which were previously the main food of hominins, have become difficult to obtain during the cooler season. Therefore, animal protein, especially during the winter months, has become a priority food source. It was a natural adaptive response to harsh environmental conditions – any organism always strives to extract the maximum number of calories from the material available to it with minimal energy expenditure. Taming fire and using it to pre-treat meat has improved the absorption of animal protein.
Physiologically, primates do not have high fat or protein requirements. The increase in the share of animal food by human ancestors speaks more about the high metabolic flexibility of primates than about the actual benefits of meat. However, increasing the proportion of meat in the diet provided additional sources of energy for the body with a larger brain. It increased the chances of survival in the face of a deteriorating food supply and, as a result, provided more profitable competitive advantages over other humanoids, allowing hominids not to leave the distance of the evolutionary marathon.
In addition, proteins provide a stronger satiating effect than carbohydrates and fats. They are digested for a long time, thus providing a long-lasting feeling of fullness, and allow you to get by with less food *. No wonder meat has become such an attractive food item.
About 800 thousand years ago, finally, modern man (Homo sapiens) appeared, for whom the consumption of a high amount of meat became the norm. The transition to new food sources required appropriate genetic adaptations associated with the metabolism of fats and cholesterol.
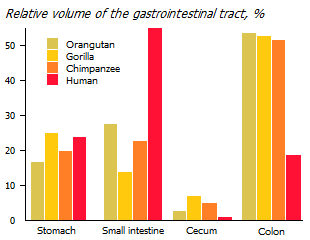
There have also been anatomical and enzymatic adaptations of the gastrointestinal tract to new food sources.
The developed large intestines that monkeys have means a large mass of satellite bacteria contained in it. The number of microorganisms colonizing the human intestine is an order of magnitude greater than the number of cells in its body, and in great apes this ratio is at least two higher. Gut bacteria produce many important nutrients from indigestible food that are either not supplied from outside or are supplied in insufficient quantities.
Due to the increase in animal protein intake, the load on the small intestine increased. And due to the decrease in the consumption of coarse fiber, the load on the large intestine was weakened. As a result of evolution, the duodenum and small intestine in humans have significantly lengthened, while the large and caecum, on the contrary, have shrunk *. At the same time, there was a fundamental reorientation of the source of certain nutrients from internal to external.
The need for more high-calorie and pre-processed foods has increased. At the same time, due to reduced fiber fermentation, short chain fatty acids (SCFA) and many micronutrients produced by the gut microflora decreased. While SCFAs can provide up to 57% of daily caloric needs in a gorilla *, they provide only 2-9% in modern humans *.
Accordingly, a person has become more dependent on the external intake of fats and certain vitamins. The first problem was partially, but perhaps not quite adequately, solved by the consumption of bone and subcutaneous fat, as well as the brain of animals obtained by hunting. And the second problem was solved by expanding the range of plant foods, which became possible to eat due to preliminary processing on fire.
Despite the epochal change in diet from primates to humans, the human body's nutritional requirements have not fundamentally changed. They are genetically determined and for this reason they are very stable. This can be seen from the fact that the ratio of macronutrients at which the risk of breast cancer is minimal is much closer to the diet of great primates than to any other diet. Perhaps the profound changes in diet occurred in too short a period compared to millions of years of hominin evolution, and there was not enough time for a fully adequate genetic response in humans.
However, individual metabolic adaptations occurred relatively quickly. Indeed, over several tens of thousands of years *, the vast majority of humans have acquired the ability to efficiently digest grains and legumes (gluten and starch) as well as the ability to digest milk (lactose) as adults. Both provided additional chances for the survival of mankind.
Nevertheless, biological adaptations still influenced the anatomy of the body more than its metabolism and the need for nutrients (both in their quantities and in their ratios). Although the proportions of the intestines differ between higher primates and humans, the enzymatic mechanisms, the general anatomy of the intestine, and the nature of the kinetics of digestion have remained very similar. Therefore, the food sources of ancient people and their ancestors can be taken as the basis for a healthy diet of modern man.
Consider the diet that accompanied mankind throughout most of its history – the Paleolithic era. It is clear that there did not exist, and could not exist, a single Paleolithic diet for all our ancestors, because food sources changed radically depending on the ecological environment, season and geographical latitude. However, there were certain dietary trends.
So, during the Paleolithic, the main food products, depending on the season, habitat and availability, were game, fish and other seafood; insects and invertebrates; nuts; seeds; fruits; leafy vegetables, herbs, tubers and roots; berries; mushrooms, occasionally – eggs and honey. At the same time, there were no such modern food products as vegetable oils, sugar and dairy products, salt, alcohol, highly processed and refined foods.
Food processing technologies were limited. Meat and tubers were baked on fire, which increased their digestibility, and hence their energy value. Other plant foods, in most cases, were eaten raw and fresh. Wild grain products were pre-milled, and legumes, which require a long time to cook when dry, were consumed immature.
The food of an ancient person was less high-calorie, but at the same time much more diverse than the food of a modern person. And the quality of the raw materials was noticeably different from the modern one. The meat of wild birds and animals was poor in saturated fats. Wild vegetables and fruits, such as wild carrots, cabbage, lettuce, plums, apples, and pears, had less sugar and more fiber, protein, and phytonutrients than the cultivars consumed today. The intake of fiber was about 100 g per day *, the main source of which was vegetables, fruits and herbs. Thus, the Paleolithic diet contained very few high-glycemic carbohydrates *.
Protein sources were mainly nuts, bushmeat and fish. Due to seasonality and limited availability of nuts and legumes, there was little vegetable protein. There was also little animal fat, so even with high cholesterol intake, cardiovascular disease apparently was not common. A favorable ω-6:ω-3 fat ratio and a high intake of natural antioxidants counteracted inflammatory processes. The low consumption of sucrose and the pronounced predominance of unsaturated fats over saturated fats also had a positive effect. The food itself was not as fatty as it has become today thanks to modern animal fattening technologies and selection work on oilseeds.
Compared to the average modern American diet, the typical Paleolithic diet contained at least 2 times more fiber, 1.5-2 times more polyunsaturated and monounsaturated fats, 4 times more ω-3 fats, and 60-70% less saturated fat. Protein intake was 2-3 times higher, potassium – 3-4 times higher; and sodium – 4-5 times lower *.
How healthy can a Paleolithic diet be called? In general, the nutritional value and calorie content were satisfactory, but they strongly depended on the season and crop. An analysis of the fossil teeth of ancient people shows that their periods of abundance were often interspersed with periods of starvation. The practice of fasting, although forced, has a longer history than we can imagine.
However, if you try to replicate the Paleolithic diet, and to do so, consume the same amount of the same food from the supermarket, this would mean a significantly higher intake of simple carbohydrates, cholesterol, fat, and in general, a higher calorie intake than ancient people. At the same time, the mineral supply may turn out to be noticeably worse than in the Paleolithic due to mineral depletion and toxic contamination of fertile soil.
In addition, diet cannot be considered in isolation from a person's lifestyle. The Paleo diet goes hand in hand with the Paleo lifestyle, with its periods of hunger, cold, and high physical activity. Paleolithic people were forced to move a lot in order to move from a place devastated by them to a new one, richer in food. The very extraction and processing of food was energy-intensive, because they required significant physical effort. Due to the fact that a significant part of the glucose was used to feed the muscle cells, taking even a large amount of carbohydrates did not cause a high level of insulin in the blood.
The next stage in the evolution of nutrition, after the development of meat, were cereals and legumes. Their cultivation, together with the mastery of cooking and other food processing technologies, allowed a person to significantly increase the calorie content of food. The transition from a nomadic to a sedentary lifestyle allowed for long-term food supplies. And the domestication of animals provided a stable source of protein. Now the fate of man depended more on his zeal, and not on the whims of nature.
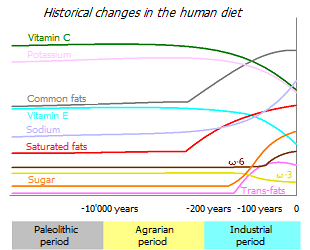
With the beginning of the agrarian revolution, human life has become more high-calorie and energetically safe. However, compared to the Paleolithic, food became less diverse, and the quality and ratio of fats in food worsened. The body's adaptation to new food and a new way of life was accompanied by a deterioration in health over many generations. In particular, with the beginning of the cultivation and selection of cereals, and the consumption of meat from domesticated animals, the average height of people has decreased, and diseases associated with a deficiency of minerals and vitamins have become more frequent *.
A new wave of food changes broke out during the colonization of overseas lands, when new plants and fruits began to enter the diet of people. Then – during the industrial revolution, when new technologies for processing food appeared. The diet of European countries changed more and more rapidly. Canned food, sugar, vegetable oils, margarine and other products that were not previously consumed appeared on sale. Food has become highly refined, ie. unnatural, depleted in valuable nutrients.
Globalization and the spirit of profit have spread this style of eating around the world. The desire to satisfy the taste buds has made it predominant. And the industrialization of agriculture and the food industry made it affordable even for the poor. The diet of modern man has become infinitely far from the diet of his ancient ancestors, and his physical activity has fallen to a historical minimum.
At present, the flywheel of the perversion of natural food has accelerated to its maximum and continues to move further. Supermarket shelves are full of unnatural, and even frankly harmful products that do not correspond to the biology of our body. Many cooking shows and sections in women's magazines can be ironically titled «How to Slowly Kill a Family and Stay Away from Suspicion.» Perhaps in a few millennia, human biology will be able to transform to today's diet. But until then, inadequate nutrition will pose a threat to our health.
We list the main dietary problems that humanity is currently facing:
1) high calorie content of food;
2) excessively high consumption of fat and sugar;
3) violation of a healthy balance of carbohydrates and fatty acids:
- imbalance simple:complex:indigestible carbohydrates to the detriment of fiber;
- imbalance of dietary fat types (saturated:unsaturated), omega-6:omega-3, short:medium:long chain, etc.;
4) the abundance of unnatural and carcinogenic substances in food, as well as dangerous food processing technologies;
5) a departure from the practice of periodic food restriction (fasting).
The modern diet does not give a person any competitive advantage. On the contrary, it directs man as a biological species towards degradation. Cardiovascular disease, obesity, diabetes, hypertension, cancer, kidney stones, Alzheimer's disease and many other common «diseases of the century» are rapidly expanding in the world. The further, the more these diseases get younger and progress.
Without a healthy diet, there can be no healthy person. What remains to be clarified is what a «healthy diet» is.
When developing a practical meal plan, nutritionists adhere to six basic principles – calories, adequacy, balance, density, moderation, and variety.
The calorie content of food, as before, remains an important requirement for it. However, in today's world, a calorie surplus is more common than a calorie deficit. Enough food is currently being produced to feed all 7 billion people on the planet. Hunger in certain regions of the planet is caused by political, not technological reasons. One and a half million are obese, and 30% of the food produced is recycled *.
The graph shown here shows the association of dietary calories with the incidence of breast cancer. The red color indicates the 10 countries with the highest incidence, and the green color indicates the 10 countries with the lowest incidence among those countries where breast cancer is the most common type of cancer. Orange indicates the 10 countries with the lowest incidence among those countries where breast cancer is not the most common type of cancer. In addition, blue indicates another 20 countries that are included in further analysis, and gray indicates countries that are not included for the sake of simplification. In the blue group were selected those countries that have the largest deviation from the average curve. Otherwise the associations would be too explicit.
The large scatter of points on the graph relative to the expected association (purple line) suggests that diet is not the only important risk factor for breast cancer. In countries with the highest incidence, there are sufficient other risk factors. Reducing or increasing the influence of these factors can significantly improve or worsen statistics. In general, it would be more correct to talk about a healthy and unhealthy lifestyle than to isolate the nutrition factor from it. Nevertheless, as can be seen from the graph, the dependence of morbidity on calorie intake remains one of the most important risk factors.
The required level of calorie intake is individual. Usually proceed from the consumption of officially recommended 32 kcal per 1 kg of body weight. Thus, the recommended calorie intake for average women would be ~ 2'000 kcal/day *. In general, the daily caloric intake should not be less than 1'600 kcal/day *, but should not exceed 2'500 kcal/day *. A more accurate daily calorie requirement can be easily calculated using ready-made applications *, since it depends on the existing body mass index, age and level of physical activity.
In almost all countries of the world, calorie intake is significantly higher than required. For example, in Europe it is one and a half times more than official recommendations. Eating too much calories has a greater impact on breast cancer risk than too little exercise *. Conversely, limiting energy intake to about a third reduces the incidence of carcinogen-induced mammary tumors in experimental animals by 90% *.
Chronic energy imbalance, in which energy intake exceeds energy expenditure, is recognized not only as a risk factor for cancer, but also as a cause of a global epidemic of overweight and obesity, cardiovascular disease, type II diabetes, non-alcoholic fatty liver disease, chronic kidney disease and accelerated aging processes.
As the graph above shows, the age-standardized incidence of breast cancer in women is directly associated with the calorie content of the food they eat. Cancer is a disease mainly of "well-fed" countries. It's fair to say that while dietary calories are the biggest contributor to lifestyle-related breast cancer risk, there are many other risk factors. However, genetic differences between different populations do not affect incidence rates.
To eliminate the most significant confounding factors, the following graph additionally adjusts for the mean median body mass index, fertility rate, and age of women at first birth in each of the countries considered. The rest of the risk factors are less influential, more evenly distributed, and, most likely, will have little effect on the final result.
After the recalculation, the vertical position of the countries has changed somewhat. The association curve became less dramatic and flatter, but the direct relationship between breast cancer risk and calorie intake remained. At the same time, the scatter of indicators relative to the averaged curve remained quite large due to the significant influence on the risk of cancer of the characteristics of the national diet, as well as due to non-dietary factors.
The minimum risk, judging by the graph, is observed when the calorie content of the diet is at the level of the physiological minimum, i.e. the lower limit of calories from food, which is enough to maintain the life of the body. Up to a level of about 2'500 kcal/day, the risk curve increases relatively slowly, but the higher the calorie content, the more rapidly it increases. An increase in daily caloric intake from 2'000 kcal to 3'500 kcal is associated with a threefold increase in breast cancer incidence.
Our bodies have evolved in a calorie-deficient environment where we had to store energy in the form of fat during good times in order to use it during bad times. Our instincts and molecular mechanisms were not ready for the fact that there will always be enough food. So people actually overeat. Current consumption recommendations are approximately 2'000 kilocalories per day, which corresponds to the minimum risk of cancer on the graph. At the same time, the actual calorie intake in European countries is on average one and a half times higher, and corresponds to the maximum risk.
Presumably, during the Paleolithic, the average calorie content of human food in favorable times did not exceed 3'000 kcal/day *, however, as we know, in those days, energy expenditure was much higher than that of a modern person in «wealthy» countries. In addition, periods of abundance of food alternated with periods of its lack. Thus, the necessary balance between the debit and credit of energy was observed in the body.
It is logical to assume that strategies that reduce the availability of energy to cells may be potentially beneficial in the prevention and treatment of chronic metabolic diseases. Such strategies can be, for example, caloric restriction of food, poor absorption of food, or a decrease in glucose metabolism. On the other hand, it is possible to increase the consumption of the received energy, for example, with the help of moderate physical activity. However, it is easier to limit the intake of calories than to get rid of those already received.
The main contributor to caloric intake, and to the risk of developing cancer in general, is dietary fat, which will be discussed in more detail below. Other main reasons for the excess caloric content of the modern diet are large amounts of food taken, large amounts of sugar, as well as alcohol. Excess calories are closely related to nutrient density.
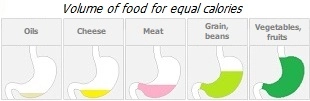
Food density allows you to estimate the concentration of the measured value per unit volume of food *.
Energy density measures the energy content in a standard weight/volume of food or drink (kcal/100g). Its value is highly dependent on the water content of the product in question. Dry foods such as cereal or dried fruit have a higher energy density than cooked cereal or hydrated fresh fruit. At the same time, vegetables rich in water and fiber have a low energy density.
The energy density of food depends on the balance of macronutrients in it. Because fat and alcohol are higher in calories than carbohydrates and proteins, increasing their share of total intake will increase the energy density of the food.
Compared to anthropoid primates, humans consume energetically denser food. Due to the low energy density diet, gorillas spend at least half of their waking time eating. A more dense food of a person allows him to free up a significant part of the time for other activities that provide the human race with progress and dominance over other biological species.
However, eating large amounts of high energy density foods easily leads to high total calorie intake, which is just not what we want. Moreover, the increase in the calorie content of food occurs mainly due to sugar and fat, which are difficult to access in nature, but are present in excess in the modern diet. It is no coincidence that in the wild, with its hunger and cold, cancer is extremely rare, while in human civilization the number of cancer cases is growing along with an increase in calorie intake.
Nutrient density measures the nutritional content of a unit of standard weight (100 g), calorie content (100 kcal), or serving size. The more nutrients a food provides relative to its calorie content, the higher its nutritional value.
Examples of nutrient-dense foods are vegetables, whole grains, low-fat dairy, seafood, lean meats, eggs, peas, beans, and nuts. Examples of nutrient-poor foods are extra sugar and sugary foods; refined flour; peeled grain; additional fats, especially refined ones.
Do not forget about the bioavailability of food products. With the same weight or volume, they can have different degrees of assimilation. Raw egg protein can be digested quickly and almost completely, while cooked egg protein is much worse. Likewise, finely ground food will be better digested than large chunks, and mushroom powder is better than chopped mushroom. Animal protein will be better absorbed than vegetable protein. Calcium from spinach will be absorbed much worse than from yogurt. Some substances are less absorbed when combined with another (for example, protein with plant polyphenols), while others, on the contrary, are better (for example, curcumin with piperine). Substances that are deficient for the body are better absorbed than those that are in excess in the body.
This means that all our preliminary estimates of the intake of certain substances into the body should be considered as approximate. How many nutrients are absorbed from any product depends on many conditions. But in any case, it will not be 100%.
The quality of food products depends on the conditions in which they were grown, harvested, transported and stored. Suffice it to recall that up to 15% of the grain crop is affected by aflatoxin, the strongest carcinogen. Most often, aflatoxin is found in the husk of peanuts.
Processing technologies also greatly influence the quality of the finished food. Cooking softens food and makes it easier to digest animal proteins and many complex carbohydrates. At the same time, heat destroys plant enzymes, essential amino acids such as lysine, and vitamins such as B1, B5, B6 and C. In addition, up to a third of the coenzyme CoQ10 is lost during frying (but not boiling)*.
High temperature processing leads to degeneration and oxidation of fats, as well as the formation of acrylamide and advanced glycation end products. All of these increase inflammatory levels and contribute to the development of a number of degenerative diseases, including the cancer * *. Therefore, the cooking methods in order of decreasing safety are as follows: steaming → baking in own juice → boiling → open baking → microwave processing → frying.
A growing body of evidence tends to suggest that at least half of all food taken by a person should come to the dining table in a raw, unheated form. Raw food includes: fresh vegetables, berries, fruits, seeds, nuts, algae; fermented foods (sauerkraut, soy or nut yogurt, live kvass, kombucha); soaked raw nuts and seeds; germinated seeds and grains; dried fruits.
Pre-soaking/sprouting grains, seeds, and nuts helps break down the phytates and lectins they contain that interfere with nutrient absorption *. For pre-soaking, seeds (chia, dill, flax, cumin, pumpkin) and nuts (almonds, hazelnuts, pecans, walnuts) are usually taken. And for germination – grain (millet, sunflower, red clover, black mustard, radish, sesame, amaranth, quinoa, broccoli) and grains (wheat, rye, barley). In this case, the material should be washed regularly to prevent the appearance of mold.
Fermenting food with bacteria and yeast improves nutrient absorption *, increases the quantity and diversity of intestinal microflora *, and stimulates the immune system *. The best known fermented foods are kvass; sauerkraut, cucumbers or watermelon; yogurt or kefir; kombucha; apple vinegar. Most often, apples, watermelons, beets, carrots, eggplant, soybeans, broccoli, ginger root, mustard greens are also fermented.
Food variety is an important principle of a healthy diet.
All foods vary greatly in their nutrient composition. For example, poppy seeds and sesame seeds contain a lot of easily digestible calcium, and are a more preferred source of this element than dairy products. Flax, ginger and chia are high in ω-3 fatty acids.
Vegetables provide us with a wide variety of plant-based nutrients. Red vegetables usually contain lycopene; yellow-green vegetables – lutein and zeaxanthin; red-violet vegetables – anthocyanides; orange-yellow vegetables – flavonoids; green vegetables – glucosinolates; and white-green vegetables are alkyl sulfides. Diversity of food therefore makes it possible to more fully ensure nutritional adequacy. Flavonoid intake is inversely associated with breast cancer risk *, especially in postmenopausal women *. And combinations of different herbal products enhance their biological effect in a synergistic way *.
For reference: modern hunter-gatherers in Australia consume about 800 types of plant foods, while in the normal diet of a modern person there are only about three dozen of them. Thus, the diet of primitive tribes is much more varied than the «Western» diet. Diversity of food products is closely related to the adequacy of food.
The adequacy of food is assessed by a sufficient level of intake of nutrients necessary for normal life. This applies not only to macronutrients (proteins, fats, carbohydrates), but also micronutrients (vitamins, minerals, phytonutrients, antioxidants, etc.).
Despite the fact that the daily calorie content in Ukraine and other European countries significantly exceeds not only the physiological minimum of 1'600 kcal, but also the recommended threshold of 2'200 kcal, it can be said that the population of these countries is undernourished, since refined and denatured food is not provide a sufficient supply of vital nutrients. At the same time, there is a monstrous imbalance between plant foods and fats in favor of the latter.
There are more than 40 essential nutrients *, the intake of which is mandatory for the body: water; carbohydrates; proteins and nine essential amino acids; EFA (essential fatty acids); vitamins – A, C, D, E, K, and eight B vitamins; as well as about 15 minerals and trace elements. For all of them, recommended intake rates (RDA) are defined.
All essential nutrients are divided into macro-nutrients and micro-nutrients.
Macronutrients are nutrients that the body needs in large quantities (tens of grams per day); mainly fats, proteins, carbohydrates and fiber. Macronutrients provide the main energy and material for the existence and renewal of the body.
Micronutrients are nutrients required by the body in small to very small amounts (milligrams and micrograms per day); this includes vitamins, minerals and trace elements.
Micronutrients are covered in more detail in the «Corrective supplements» section †, but we'll look at macronutrients for now.
Fats. The physiological need for fat for women is 60 g/day *.
Each fatty acid consists of three structural parts. At one end is a carboxyl group. It is followed by the «fat» part of the molecule, consisting of a chain that can contain from 2 to 22 or more carbon-hydrogen units. It is closed by a methyl group at the other end of the molecule. Depending on the length of the hydrocarbon chain, fatty acids are classified into short chain (less than 6 carbons), medium chain (6-12 carbons), long chain (13-21 carbons) and extra long chain (more than 21 carbons).
Fatty acids with one or more double carbon bonds are called unsaturated because some of the double carbon bonds are not saturated with a hydrogen atom, and fatty acids without double carbon bonds are called saturated because they are fully saturated with hydrogen atoms.
When an unsaturated fatty acid molecule has one double carbon bond, it is considered monounsaturated, and if more than one, it is considered polyunsaturated. Molecules of polyunsaturated fatty acids can have a trans configuration (when the molecule is straight), or a cis configuration (when the carbon-hydrogen chain is bent). Trans fats are biochemically more inert than cis fats.
In polyunsaturated fatty acids ω-3, the first carbon double bond falls on the third carbon atom from the methyl end, in ω-6 – on the sixth, and in ω-9 – on the ninth. The specific location of this double bond in the carbon-hydrogen chain affects the degree of its participation in a particular biochemical reaction and, as a result, the risk and course of the disease.
Dietary fats are important not only as a source of energy. Fatty acids are constituents of the cell membranes of all body cells. As a result of the metabolism of fats, many bioactive lipid molecules are formed, which are indispensable for cell membranes, or participate in the life of cells in various ways. These molecules have biological activities that affect metabolism, cell and tissue function, and their response to hormonal and other signals.
Disturbances in lipid metabolism can lead to disruption of signaling networks, to a change in the chemical composition of the membrane and, as a result, to a change in its fluidity and permeability. In conditions of excess nutrition, fat entering the cells is not converted into energy, but accumulates inside. The health of the mitochondria of cells (and the whole cell as a whole) worsens from this, which, in turn, increases the risk of many pathological conditions.
Fatty acids help to adequately absorb fat-soluble substances from food, including vitamins A, D, E and K, as well as calcium *. At the same time, many dietary fats allow gut bacteria (and endotoxins) to enter the bloodstream, which increases systemic inflammation, lowers immunity, and increases cancer risk *. In addition, fatty acids activate the fat receptor (fatty acid translocase, CD36), which promotes cancer cell metasis *.
Until now, it was believed that for cancer cells, the main raw material for energy production is glucose. But in recent years it has become clear that many cancer cells are able to resort to the use of other sources, including fats. In terms of breast cancer risk, dietary fat appears to pose a greater threat than protein and carbohydrates *, and excess intake may have latent and long-term effects. Although fatty acids cannot be used as a primary fuel in cancer cells with a mitochondrial defect, they can enhance their glucose fermentation *.
A special dietary study of 88 countries on five continents that assessed the association of total fat intake with breast cancer incidence found a statistically significant (0.6) correlation between average fat intake and overall incidence. Even after adjusting for confounding factors, there was a strong moderate to strong correlation between total fat intake and breast cancer incidence *. The graph below confirms this relationship. In studies of this kind, concomitant factors introduce a certain error, but case-control studies confirm the noted association * *.
A high fat diet increases visceral adiposity (around internal organs) compared to a low fat diet, even with the same calorie content of both diets; at least this has been observed in experimental animals * *.
High fat intake increases overall inflammatory levels *. First, it is the result of cross-species changes in gut bacteria that lead to the activation of pro-inflammatory pathways. Secondly, dietary fat promotes the movement of microbial products and liposaccharides from the intestines into the bloodstream (liposaccharides are also a powerful stimulant of inflammatory reactions).
Of course, the incidence of tumors is directly associated with the total caloric intake of food, regardless of the level of dietary fat in it *. However, fat, due to its high energy density, is the largest source of calories in food.
The association of fat intake with breast cancer risk has been the subject of many studies. Unfortunately, the vast majority of them did not take into account the composition of fats consumed and the context in which they are consumed, which was probably the reason for ambiguous, sometimes even contradictory conclusions *.
According to the World Health Organization (WHO) and the Food and Agriculture Organization of the United Nations (FAO), for a healthy adult population, dietary fat should provide 15-35% of all food energy *. However, the graph above suggests that exceeding 25-30%E already dramatically increases the risk of breast cancer.
Earlier observational studies of breast cancer incidence and mortality rates in different countries correlated with total dietary fat rather than with any specific type of fat *. However, recent experimental data show that, given the same calorie content of the diet, the dietary fat class can influence carcinogenesis no less strongly than the total fat content in the diet *.
The type of dietary fat is fundamentally important in tumor development * because different fatty acids have different effects on cell membrane properties and have different effects on signaling pathways involved in cell proliferation * *. A special meta-analysis on the effect of fat on breast morbidity concluded that premenopausal mixed fats have little effect, but even within the same family, lipids may have different effects *. In other words, the formula of a fatty acid is crucial in assessing its benefits or harms: different classes of fatty acids can either promote breast cancer or protect against it *. Let's consider this in a little more detail.
PUFAs (polyunsaturated fatty acids) make up the majority of all fats in popular vegetable oils such as sunflower, corn, soybean and cottonseed. Because of their unsaturation, polyunsaturated fatty acids are more reactive than saturated fatty acids and are more likely to react with other metabolically key molecules
The high reactivity of these fats, however, causes them to oxidize fairly quickly to form toxic products, especially in the presence of heat and light. When oxidized, they produce free radicals that contribute to tissue damage, inflammation, and the associated risk of tumor development. Thus, an increased intake of PUFAs requires a corresponding increase in the dietary antioxidants found in vegetables, which is not normally met in the modern Western diet.
Different types of PUFA have different carcinogenic effects. A high intake of PUFA ω-6 has been associated with an increased risk of breast cancer * *, and a high intake of marine PUFA ω-3 has been associated with a marked reduction *. This is partly because ω-3 and ω-6 saturated fatty acids (and their metabolites) express genes associated with a wide range of biological functions, including nutrition, division, cell proliferation, metastasis, factors transcription, autophagy, etc.
Looking ahead, we note that both ω-3 and ω-6 are essential fatty acids, and it is important here not only to reduce their total intake, but also their ratio in the food consumed. Due to the fact that the same enzymes are involved in their metabolism, both of these fatty acids «compete» for common resources. Therefore, the greater the saturation with ω-3 acids, the less the negative effect of ω-6 acids. However, there is a certain limit here as well.
A reconstruction of the putative Paleolithic diet estimated long-chain PUFA intake at ~20 g/day, of which three-quarters came from plant sources. The intake of linoleic acid is estimated at 8.8 g/day, and α-linolenic acid is approximately 12.6 g/day. Intake of eicosapentaenoic acid (EPA, ω-3) is estimated at 0.39 g/day, and docosahexaenoic acid (DHA, ω-3) is estimated at 0.27 g/day, and the ω-3:ω-6 ratio is ~1.4 *.
Interestingly, increasing dietary ω-3 (which automatically increases the ω-3:ω-6 ratio) has been shown to reduce the risk of breast cancer even in the offspring of experimental animals. The next generation of female mice fed a diet enriched with flaxseed oil or fish oil experienced later puberty and their mammary glands contained fewer targets for malignant transformation *.
It is assumed that the ω-6 level required to prevent symptoms of essential fatty acid deficiency is 1.5-2% of total daily energy intake (%E) for both adults and children * *. Thus, increasing PUFA ω-6 intake above 3%E not only makes no sense, but also begins to pose a potential health hazard.
On the other hand, increasing the concentration of EPA and DHA in red blood cells to 10% of total fatty acids provides a cardioprotective effect *. And from such an indicator we should also expect benefits for other organs, and the entire body as a whole. If we assume an adequate consumption level of 3 g of EPA and DHA per day, then to ensure such a concentration of EPA+DHA, the daily fat intake can be represented as 10-12 g of fish oil and 20 g of other fats. Since such a diet seems difficult to achieve, supplementation with EPA and DHA makes sense.
MUFAs (monounsaturated fatty acids) are found in significant quantities in vegetable oils. Meanwhile, their impact on breast cancer risk is unclear, and their safe consumption threshold is unknown.
In a meta-analysis examining colorectal cancer, PUFA ω-3 EPA and DHA were associated with an 11-12% reduction in risk, and linoleic acid was associated with a 19% increase in risk; other fats had no significant effect on disease risk *. A meta-review examining the effect of different classes of fatty acids on pancreatic cancer found an inverse association of incidence with MUFA (relative risk ~0.9) and a direct association with SFA (relative risk ~1.13) *. However, according to a meta-review examining breast cancer, the relative risks for the highest and lowest categories of serum SFA, MUFA and PUFA were 1.00, 1.41 and 0.59, respectively *.
It has also been reported that MUFAs may have a protective effect in premenopausal * but not menopausal women *. In postmenopause, consumption of total MUFAs, especially myristoic acid and erucic acid, has been associated with an increased risk of breast cancer *. This uncertainty makes it difficult to evaluate the benefits or harms of MUFA relative to other classes of fatty acids.
Although many studies have suggested a beneficial role for MUFA-rich olive oil in reducing the risk of breast cancer, this is most likely due to the plant nutrients in olive oil rather than the MUFA (oleic acid) itself *.
SFAs (saturated fatty acids). In a meta-analysis of prospective studies, the relative risk of postmenopausal breast cancer was more pronounced for increased intake of saturated fat (SFA) than for polyunsaturated fat (PUFA) *. Particularly strong associations were observed for SFAs *.
It is estimated that reducing postmenopausal SFA intake to 9%E may reduce the risk of breast cancer in postmenopausal US women by 10% *. Given that precancerous changes occur over many years, it is hardly worth attributing this risk exclusively to postmenopausal women. Perhaps in postmenopausal women we are already seeing the result of the chronical high consumption of SFA in previous years.
An increase in saturated fat intake was positively correlated not only with an increased risk of breast cancer *, but also with a worse prognosis for patients *. The difference in mortality rates between the groups with the highest and lowest consumption of saturated fat in individual studies was up to one and a half times. But since all of the cases mentioned above were samples of a typical Western diet, the SFAs in question appear to have consisted of animal fats rather than vegetable fats.
Saturated fat's bad reputation led the US National Research Council to recommend in 1989 that SFA be reduced to 10%E in order to prevent cardiovascular disease and cancer *. In recent years, there have been proposals to replace the long chain SFAs found in animal foods (animal fat, tallow) with medium chain SFAs found in plant foods (coconut oil).
There are reasonable theoretical justifications for this proposal. Long-chain SFAs induce inflammation by partially mimicking the action of bacterial lipopolysaccharides (endotoxins) *. Medium chain SFAs produce fewer oxidative molecules and therefore produce less inflammation. In addition, they form ketone bodies more easily, so they appear to be preferable to long chain SFAs *. However, there is as yet no conclusive clinical evidence in favor of medium chain SFAs.
Under the condition of healthy physiology, an increase to a certain limit of SFA consumption does not cause a pathological change in their concentration in tissues, since fats are successfully metabolized. However, this homeostatic balance can be easily disturbed by a high calorie intake and a sedentary lifestyle, contributing to the excessive accumulation of fat in the tissues *.
TFAs (trans fatty acids) produced by the partial hydrogenation of vegetable oils (eg margarine) have been associated with an increased risk of breast cancer * *. Only natural conjugated linoleic acid (CLA) has shown anticancer properties in some studies * *.
The American Cancer Society and the American Society of Clinical Oncology recommend minimizing your intake of saturated and trans fats *.
Increased consumption of trans fats worsens most health indicators, including an increased risk of depression * *. The World Health Organization recommends that total trans fat intake should not exceed 1% of total energy intake (< 2.4 g) *. Because these amounts are readily acquired from latent fat in food (mainly meat), any additional intake of TFA, such as found in margarine or animal fat, would be excessive.
So, different dietary fats have different effects on tumor processes. Although the findings of many studies are often conflicting, it has been noted that an increased risk of breast cancer is more associated with artificial trans fats * than with saturated fats *. Also, this risk is more associated with vegetable oils rich in PUFA ω-6 linoleic acid (sunflower, soybean, corn oils) than with vegetable oils rich in MUFA ω-9 oleic acid (olive and canola oils, avocado) * *.
A meta-analysis of the composition of fatty acids in biological samples found a significant protective effect for PUFA ω-3 acids, while MUFA ω-9 oleic acid and SFA palmitic acid, on the contrary, were significantly associated with an increase in the risk of breast cancer *. Linoleic acid in vitro was significantly more toxic to immune cells (T lymphocytes) than oleic acid * * *.
In experiments with rats, mammary tumors grew faster when the proportion of corn oil (rich in PUFA ω-6) was increased in the diet than when the proportion of coconut oil (rich in medium-chain SFAs) was increased in the diet. At the same amount of fat in the diet (20% of the feed weight), with an increase in the proportion of linoleic acid, the risk of cancer steadily increased. And when reaching 4.4% linoleic acid from the weight of the feed, it was assumed that the maximum carcinogenic response would be achieved *.
With little difference in calories, a diet high in seed oil (safflower or corn) increased the incidence and rate of development of mammary tumors in rats compared to a diet high in fruit oil (olive or coconut) *. Linoleic acid dominated in safflower and corn oils (82% and 56%, respectively), while oleic (79%) and myristic (54%) acids dominated in olive and coconut oils.
In other manipulation studies, given the same calorie intake, high fat intake in the form of linoleic acid was also associated with higher incidence and shorter latency of mammary tumor development in mice * and rats *. In all the five studies discussed above, the tumor was provoked by a chemical carcinogen, and the caloric content of the animals' diet was not limited.
A diet containing 3% by weight sunflower oil (PUFA ω-6) in one subgroup of rats and a diet containing 20% tallow or coconut oil (SFA) in another subgroup increased tumor rates in rodents with approximately equal success. However, it was enough to replace only 3% of tallow or coconut oil with sunflower oil in the diet of the second subgroup, as the animals developed at least twice as many tumors *.
In a study of young piglets, one group was fed the amount of linoleic acid needed to prevent deficiency (1.2%E) and the other group was fed an amount of linoleic acid equivalent to that of a Western diet (10.7%E). In the first group, piglets had healthy, normal brain development, while in the second group, neurological development was impaired and altered *.This is not a surprising result when you remember that the brain is 60% fat.
These preclinical results suggest that PUFA ω-6, especially linoleic acid, may pose a greater risk than SFA; at least when eating without calorie restriction. A special systematic review confirmed that the replacement of saturated fats with polyunsaturated fats is associated with an increase in all-cause and cancer mortality *.
Of course, the results of dietary experiments with animals cannot always be adequately projected onto humans. And it is impossible to carry out experiments on humans, similar to those carried out on rodents, because of their unethical nature. In the same time, observational studies have a different methodology, give conflicting conclusions, and often do not note the harmful effects of linoleic acid. This apparent difference in results can be explained by the fact that the diets of most countries of the world contain too much linoleic acid (~ 6%E) * for minor dietary changes to affect the carcinogenic effect. Therefore, in observational studies of human populations, positive correlations between fat intake and morbidity/mortality from breast cancer will be observed not from the type of dietary fat, but from its amount *.
The issue of linoleic acid was not an issue just a 100-150 years ago, when it was consumed primarily in whole foods rather than as a refined product as it is today. Accordingly, the amount of linoleic acid consumed was very low. Since then, global production of vegetable oils rich in PUFA ω-6 has skyrocketed and continues to grow at an alarming rate.
Linoleic acid intake in the US has increased over the past century from an adequate 2.8%E to a more than dangerous 7.2%E, while EPA and DHA intakes have declined. These changes are directly correlated with an increase in diseases such as arthritis, obesity, diabetes, Alzheimer's and cancer. In itself, such an association would not be evidence of the dangers of linoleic acid, if it were not for the above-mentioned animal experiments suggesting just such a conclusion.
At the same time, in the so-called «Blue Zone», i.e. places with the best indicators of longevity and long-term health, the consumption of linoleic acid is significantly lower than its consumption in «wealthy» countries. For example, in Icaria, the only dietary fat is olive oil, which accounts for ~6% of the daily food intake, corresponding to ~12%E as olive oil, or less than 2%E as linoleic acid *. Of course, although such a comparison is not direct evidence, however, it once again reinforces the assumptions made above.
In an eight-year clinical study involving more than 800 people, the experimental group consumed 14.8% E from linoleic acid compared to 3.9% E in the control group. Over the five years of the experiment, in people following a diet high in linoleic acid, the level of linoleic acid in adipose tissue increased from the original 10.9% to 33.7%. At the same time, members of the experimental group were 82% more likely to die from cancer compared to the control group. Even though they smoked half as much, consumed less trans fat and more PUFA ω-3 and vitamin E *.
In addition to linoleic acid, other fatty acids were noted for their negative. In postmenopausal women, MUFA myristoleic acid, SFA palmitic, palmitoleic and margaric acids, and trans fats are associated with an increased risk of breast cancer, while PUFAs eicosapentaenoic (EPA) and docosahexaenoic (DHA) acids are associated with a reduced risk *.
In general, consumption of trans fatty acids, saturated fatty acids, animal-derived monounsaturated fatty acids, α-linolenic and arachidonic acids were also associated with higher overall mortality. And consumption of marine ω-3 PUFAs and replacement of SFAs with plant-based MUFAs or linoleic acid have been associated with lower overall and cause-specific mortality * *. As you can see, researchers do not have a clear answer to the question of which is more dangerous – SFA or MUFA.
Compared to non-tumor cells, the content of pro-inflammatory arachidonic acid in the membranes of cancer cells is significantly increased – it makes up to 40% of all fatty acids of the cell membrane. Consumption of animal fats and vegetable oils ω-6 increases the content of arachidonic acid in cell membranes, especially in cancer cells *. Reducing the intake of the latter may be an attractive target in an overall cancer control strategy.
On the other hand, EPA and DHA fatty acids impair the availability of arachidonic acid, as well as reduce NF-κB activation and signaling, resulting in a reduced inflammatory response *. There have been several well-controlled studies showing that EPA and DHA intake at doses of 1.2 to 6 g/day reduce circulating inflammatory markers such as CRP, IL-6 and TNF-α * * *. The anti-inflammatory effects of EPA and DHA are not limited to blood markers. In people with type II diabetes who received 1.8 g/day of EPA and DHA for 8 weeks, there was a decrease in the expression of inflammatory genes in white adipose tissue *, which may also help reduce systemic inflammation. Longer use of EPA and DHA results in better performance *. Higher EPA and DHA, and especially DHA, are associated with a reduced risk of both cardiovascular disease and all-cause mortality *.
Of course, fatty acids in the body are capable of being converted from one to another, and the harm of certain fatty acids may be associated precisely with a violation of the healthy metabolism of fatty acids. But this topic is too complex to draw any practical conclusions from it. It is much easier to influence the quantity and quality of fatty acids through diet.
Since there is a conditional division of dietary fats into «good» and «bad», there is a lot of controversy regarding the consumption of certain sources of fats and fat-containing foods. As can be clearly seen in the graphical comparison of the composition of various fat sources, any fat source does not exclusively contain any particular fatty acid, but is a diverse mixture of fatty acids *. In each source, «good» and «bad» fats are in different combinations.
However, when choosing a source of dietary fat, it is recommended to give preference to such «healthy» fats as α-linolenic acid from the ω-3 group (linseed oil), DHA and EPA from the ω-3 group (fish oil), γ-linolenic acid from the ω-6 group (hemp oil), oleic acid from the ω-9 group (olive oil).
Medium chain fatty acids (MCFAs) are more readily metabolized to short chain fatty acids than long chain fatty acids. Therefore, it is often recommended to include coconut and palm kernel oils in your diet as a replacement for long-chain acids, since they contain relatively higher amounts of MCFAs. However, in absolute terms, medium-chain fatty acids in these sources contain little, in contrast to long-chain fatty acids (lauric and myristic). That is, the practical benefit of such advice looks small.
In addition to the classification of fatty acids by saturation, there is also their classification by the length of the hydrocarbon chains.
LCFAs (long-chain fatty acids) are mainly those PUFA, MUFA, SFA and TFA, which were discussed just above.
MCFAs (medium-chain fatty acids) are found in large quantities in coconut oil and palm kernel oil (more than 50%). In addition, they can be found in cow's milk (4-12% of all fatty acids present in it).
Compared to LCFA, MCFA is metabolized faster, more efficiently, and requires fewer enzymes and proteins involved in the process. In general, free MCFAs are more easily utilized, have a higher propensity to oxidize, and behave metabolically more like glucose than fat *.
However, the effects of different MCFAs on the body differ from one another. For example, both 12-chain lauric acid (from palm kernel and coconut oils) and 16-chain palmitic acid (from palm oil) are saturated MCFAs. However, in mice, increasing lauric acid intake resulted in greater gains in visceral fat, but smaller increases in inflammatory and liver damage markers compared to increasing palmitic acid intake *.
There are mixed reports regarding their effect on cholesterol levels. In one study, in healthy volunteers, a diet rich in lauric acid increased serum total cholesterol concentrations more than a diet rich in palmitic acid when compared with a diet rich in oleicacid *. In another study, in contrast, palmitic acid increased total and LDL cholesterol concentrations more than lauric acid relative to a diet rich in oleic acid *. In a third study, on an isocaloric diet, longer chain fatty acids provided lower serum cholesterol concentrations than shorter chain fatty acids *.
It appears that the situation with fatty acids is similar to that with carbohydrates: in general, the shorter the molecule, the faster it is metabolized after ingestion. This means that shorter chain acids saturate the blood with triglycerides faster *.
SCFAs (short-chain fatty acids) can either come from outside (import fat) or be produced inside the body (domestic fat). In the latter case, fatty acids are produced from indigestible dietary fiber by certain types of bacteria that colonize the colon. SCFAs are best sourced from resistant starches (whole grains, legumes, unripe bananas, boiled potatoes); pectin (apples, apricots, berries, carrots); fructooligosaccharides, abbreviated as FOS, inulin (Jerusalem artichoke, onion, wheat, rye, asparagus); guaran.
It is estimated that bacteria can produce ~ 15-30 grams of SCFA per day as waste products of their metabolism, of which ~ 10-15% (1.5-4.5 g) is butyrate.
Butyrate not only provides energy for colon cells, it also exhibits anti-inflammatory effects. First, it suppresses inflammation in vitro by reducing the ratio of pro- and anti-inflammatory cytokines (IL-12 and IL-10, respectively) * *.
In addition, butyrate can reduce inflammation by enhancing the activity of immune regulatory T cells (Tregs) *.
It appears that SCFA is the most attractive type of fatty acid. However, the level of their intake into the body depends on the volume of the corresponding intestinal bacteria, and this, in turn, depends on the volume of fiber supplied with food. Only a very small amount of SCFA comes from food in its prepared form (in vinegar, fermented vegetables and butter). At the same time, MCFA and LCFA, on the contrary, come exclusively from food, and usually in excessively large quantities, creating an unhealthy imbalance.
African Americans in the US and rural Africans in the Africa, despite having a common genetic heritage, have a very high difference in the incidence of colon cancer. To determine the influence of diet on this fact, a special cross-sectional manipulation study was conducted. One group of healthy people received a high-fiber, low-fat diet, while the other group received a high-fat, low-fiber diet. When both groups of subjects were changed the composition of the food, they simultaneously changed in some places the state of intestinal health. A high-fat, low-fiber diet for just 2 weeks resulted in an increase in cancer biomarkers and a switch to a more cancer-friendly gut bacterial profile; and vice versa *.
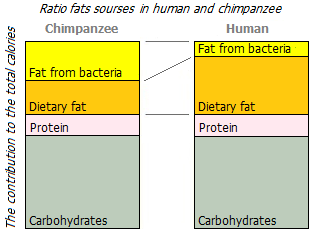
Interestingly, wild chimpanzees eat ~ 50g of dietary fat per day, mostly polyunsaturated ω-3 and ω-6 fatty acids *. And at least the same amount of fat (in the form of SCFA) they acquire «on the spot», as a result of the enzymatic activity of colon bacteria. And people in «wealthy» countries eat 120-160 g of dietary fat per day, mostly saturated with MCFA+LCFA. And they receive from bacteria, as a maximum, 35 g of SCFA. As you can see, the ratio of SCFA to MCFA+LCFA in chimpanzees is many times better than in modern humans.
Of course, in humans, the relative length of the large intestine is 2.5 times shorter than in chimpanzees. This means that there is much less room in it to house the gut bacteria that produce SCFA. But perhaps even the current volume would be enough to produce enough SCFA if the human diet were close to the vegetarian diet of the chimpanzee. In fact, people on a «Western» diet consume ~ 25 g of fiber per day versus ~ 200-220 g consumed by chimpanzees. And in no country in the modern world does the average daily intake of fiber exceed 50 g, which is half that of primitive people.
From all this analysis of the impact of the quality of dietary fats on human health, a very important conclusion can be drawn:
In fact, the current recommendation to consume less dietary fat and more fiber-rich foods (vegetables, legumes, and whole grains) is nothing more than an unconscious suggestion to increase the ratio of short-chain fats to long-chain fats.
It seems that the effect of saturated and unsaturated fats is more complex than previously thought and depends on many factors (age, menopausal status, body mass index, baseline ratio of different types of fats, dietary calories, alcohol, other dietary components, fat molecule formula, etc.). In addition, the consumption of certain fatty acids is not equivalent to their accumulation in cells or tissues. Some fatty acids can be metabolized in the body into other fatty acids. This makes it difficult to assess the benefits of consuming each of the fatty acids.
The balance of fatty acids is no less important than their absolute values. Most often, attention is paid to the ratio of saturated:monounsaturated:polyunsaturated fats (SFA:MUFA:PUFA) and polyunsaturated ω-3:ω-6. In the top ten most disadvantaged countries for breast cancer, the ratio of SFA:MUFA:PUFA is 1:0.8:1.6 *.
The graphs shown here show the incidence of breast cancer as a function of dietary fat ratios SFA:(MUFA+PUFA) and MUFA:PUFA. Since the incidence rate is strongly influenced by the total calorie content of the diet, to reduce the influence of this factor, only countries with similar high caloric values (from 3'000 kcal and above) were compared here.
In the first graph, the association of cancer risk with an increase in the SFA:(MUFA+PUFA) ratio can be clearly seen. The more saturated fats relative to unsaturated fats, the worse. But on the second graph, there is no need to talk about a direct association. This may be due to the fact that general unsaturated fats were taken into consideration, while it is known that their varieties can play a different, often opposite role.
The current recommendation for the ratio of SFA:MUFA:PUFA in the diet of a modern person, proposed by cardiologists, is 1:(1,3-1,5):1 *. Based on the first graph, the risk of breast cancer is also low with this ratio, about the same as in China or Greece. In the gorilla diet, the ratio of SFA:(MUFA+PUFA) comes to about this level (1:2); and the MUFA:PUFA ratio is ~ 1:4.5 *. In Upper Paleolithic humans, the SFA:PUFA ratio was supposedly 1:1.4 *, while the median SFA:PUFA ratio in European countries was 1.9:1 *, i.e. twice the current recommendation, and almost three times the Paleolithic level.
Modern hunter-gatherer tribes, as in Paleolithic times, have higher levels of animal fat in their diets than recommended. However, they have a lower prevalence of «diseases of civilization» * and breast cancer than white people living in the same region *. A possible reason for this paradox could be that their diets, which are relatively high in unsaturated fatty acids, are very low in ω-6 fatty acids, and have a high ω-3:ω-6 ratio. This is directly related to the difference in fat profile between wild and farm meats.
A chronically low ratio of PUFA ω-3:ω-6 in the diet leads to the accumulation of ω-6 in adipose tissue and disrupts their natural ratio in cell membranes, thereby impairing the functioning of cell membranes. However, it makes no sense to graphically analyze the relationship between cancer risk and the ω-3:ω-6 ratio among the countries under consideration, because in almost all of them the ratio is many times lower than the «healthy» value.
With the same intake of total fats, increasing the proportion of PUFA ω-3 by decreasing the proportion of PUFA ω-6 reduces the risk of degenerative diseases. In free-living higher primates, the ratio of ω-3:ω-6 in the food consumed is ~ 1:1.4 * *. In the diet of hunter-gatherers, it could be from 1:1 to 1:4 *. To be considered «healthy», the ratio ω-3:ω-6 should be kept within 1:2-1:3 *, however, the current average median ratio in most «wealthy» countries is ~ 1:20. For example, in meat from wild and grass-fed animals the ratio ω-3:ω-6 is approximately 1:2, while in grain-fed meat it deteriorates to 1:9. A meta-analysis on the relationship between the ratio and breast cancer concluded that increasing the ratio of consumption of ω-3:ω-6 in the diet of a modern person will contribute to the prevention of the disease *.
Indeed, the so-called the «Mediterranean» diet, despite its abundance of olive oil, is usually associated with a lower risk of disease than the usual «Western» diet with a predominance of saturated fats and PUFA ω-6. Olive oil is known to have a very low ω-6 PUFA content, an excellent ω-3:ω-6 ratio (1:2) and a low saturated fat content, unlike most other cooking vegetable fats.
In the previous two graphs, we compared the effect of fat ratios within disadvantaged countries on breast cancer risk. Now let's see how fat consumption differs between prosperous and disadvantaged countries.
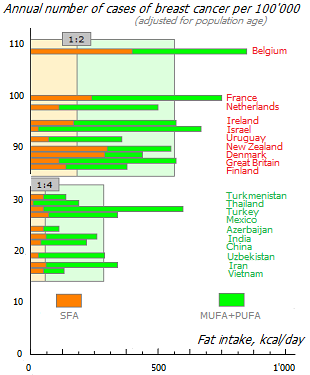
The histogram shown here clearly demonstrates the association of breast cancer incidence with the consumption of various types of fats. At the top of the graph are the ten countries with the highest incidence, and at the bottom are the ten countries with the lowest incidence among those countries where breast cancer is the most common type of cancer. In «cancer-prone» countries, both the amount of total fat and the ratio of saturated to unsaturated fats are higher. The last indicator differs between these groups by 2 times.
Among the countries where breast cancer is the leading type of cancer, the ten most disadvantaged countries have an average median ratio of vegetable fat to animal fat of 2:1. And in the ten most prosperous countries it is 4:1. At the same time, in the top ten countries with the lowest incidence of all types of cancer, this ratio is even higher – 7:1 †. The greater the predominance of animal fat over vegetable fat, the higher the risk of any type of cancer.
Despite such a large difference, these comparisons can hardly be called correct, because in a well-off group of countries, consumption of not only fats is lower, but also calories, processed meat, eggs and milk, and fiber intake is higher. So, in fact, we're not just comparing different fat intake profiles, but different dietary profiles. However, the amount of fat is the main difference between these profiles.
Saturated fatty acids (SFAs) increase blood cholesterol levels, unlike monounsaturated (MUFA) and polyunsaturated (PUFA) fatty acids. So a relatively high fat intake is acceptable without significant deterioration of the plasma lipid profile * assuming low total calories, adequate MUFA and PUFA intake * *, and a favorable ω-6:ω-3 PUFA to MUFA:PUFA ratio *. The lower the ratio of SFA:PUFA, the less negative impact on the level of cholesterol (LDL) in the blood has cholesterol coming from food. On a diet with an SFA:PUFA ratio of 1:2.5, consumption of even 6 eggs per day did not cause significant changes in LDL levels in the subjects *.
The ratio of short chain fats to medium chain fats (SCFA:MCFA), and medium chain fats to long chain fats (MCFA:LCFA) may be even more important than the ratio of saturated fats (SFA) to unsaturated fats (MUFA+PUFA). The shorter the fatty acid molecule, the less oxidative damage and inflammation it produces *, the better the cells' glucose tolerance, the less muscle fat accumulation and the more efficient mitochondrial respiration *.
From this point of view, short-chain fatty acids produced by intestinal bacteria from fiber (domestic fat) are much healthier than long-chain fatty acids obtained from animal foods (import fat). As just discussed above, the ratio of domestic:import fats in chimpanzees is ~ 1:1, while that of humans on a modern «Western» diet is ~ 1:4. In addition, import fat in chimpanzees is dominated by MUFA and PUFA, while in humans, a significant proportion is SFA. We can correct this imbalance by taking butyrate, but it is much more natural to do this by increasing your vegetable intake.
The degree of purification of consumed vegetable oils is another important criterion for their «usefulness». Unrefined oils of the first cold pressing (brand extra virgin) have a richer phytochemical composition than refined or extracted under high temperature, and because of this they are more useful.
For example, pure oleic acid (the main component of olive oil) can stimulate the growth of cancer cells in vitro *. However, the consumption of unrefined olive oil reduces the risk of breast cancer * * * due to the fact that it contains, in addition to oleic and other MUFAs, a rich variety of phenolic compounds, including simple phenols, aldehyde secoiridoids, flavonoids and lignans * *, which have antitumor activity.
When mice were inoculated with breast cancer stem cells exposed to secoiridoids, 20% of the mice did not develop tumors, and in 80% of cases, the tumors were 15 times smaller and grew much more slowly *. The prospective Epi-GEICAM study, based on 1'017 cases of invasive cancer, concluded that extra virgin olive oil taken in an amount of ≥ 2 tbsp. per day was associated with a 29% reduction in breast cancer risk compared to other cooking oils *.
Women with the highest level of olive oil consumption are almost twice as likely to get breast cancer compared to women with the lowest level of olive oil consumption * *. This is not surprising, because olive leaf extract, which contains a similar composition of phytonutrients, also exhibits a pronounced antitumor effect.
These observations suggest that the benefits of olive oil polyphenols may outweigh the harms of linoleic acid and the excess calories derived from it. However, it is impossible to say the same for all vegetable oils.
Presumably, some other unrefined vegetable oils may produce beneficial effects through other specific phytonutrients. With few exceptions, it is phytonutrients, not fatty acids, that make a particular vegetable oil healthy. By themselves, vegetable oils are refined, that is, unnatural food products.
The culinary processing of oils and fats also greatly affects their quality. The less saturated fatty acids, the more reactive they are, the sooner they are oxidized. Probably everyone knows the disgusting taste of rancid fish oil. Other unsaturated fats spoil a little more slowly, but with the same inevitability. The degree of oxidation of fats is highly dependent on light, the abundance of oxygen, shelf life, and especially on temperature. Therefore, the temperature treatment of oil (for example, frying on it), and even more so for a long treatment, especially contributes to this process.
In addition to oxidation, fatty acids undergo degradation as well as conversion to other types of fafs. Heating edible fats to normal cooking temperatures (≤ 200 °C) has minimal effect on trans fat formation, while raising the temperature further to 240 °C or more increases levels significantly *. To reduce fatty acid degradation, frying foods is best done with saturated fats that have a higher smoke point, such as lard. The fact that such fats in food are best avoided has already been noted. Accordingly, the amount of fried food should also be kept to a minimum.
If the heat treatment is carried out using vegetable oils, then in this case it is better to take their varieties that produce less carcinogenic products. When heated to 200 °C, corn, coconut and olive oils emit more particulate matter (smoke) than soybean, canola, peanut and safflower *. And when heated to 240 °C, peanut, rice, rapeseed and olive oils produce the largest emissions, while sunflower, soybean and corn oils produce the smallest ones *.
All of the above also applies to fried foods that contain fat, such as seeds, nuts or peanuts, because. the processes of oxidation, decomposition and transformation of fats can occur even inside them.
Metabolic differences between people are another issue that influences dietary recommendations for certain types of fats. In fact, there are only two truly essential 18-chain fatty acids that are widely distributed in food. They are linoleic acid (LA) with two double bonds and α-linolenic acid (ALA) with three double bonds. With the help of appropriate enzymes in the body, other long-chain fatty acids are synthesized from them, such as PUFA ω-3, such as EPA and DHA *.
The activity of these enzymes in different people is not the same, which has a genetic or epigenetic cause. Thus, for some people, it is more beneficial to get certain fatty acids from food already prepared than to rely on their internal production from precursor acids. It is for this reason that fish oils generally perform better than flaxseed oil in studies.
The amount of fat in food is undoubtedly the most controversial issue. A large study of more than 188'000 participants showed that dietary fat intake was directly associated with the risk of invasive postmenopausal breast cancer *. Increasing fat intake raises pro-inflammatory markers in the same way as increasing simple carbohydrate intake *.
Contrary to current WHO recommendations to obtain up to 30% of total daily calories from dietary fat, the results of not only observational, but also manipulative studies – both in animals * *, and in humans * * *, indicate that a safe level of fat in total calories closer to 15-20%, but not lower than 15%. A further reduction in fat intake begins to play a negative role * *. An adequate caloric diet providing less than 30% of energy from fat is sufficient to ensure normal growth and normal puberty *. By comparison, in higher primates in the wild, dietary fat typically provides ~ 14-17% of total calories * *.
In experimental mice on an unrestricted diet and an isocaloric diet, with variations in the proportion of fat in total calories from 10% to 40%, a plateau in tumor incidence was observed when reaching a level of 22%E. And in subgroups that received 10-16% of energy in the form of fat, the incidence, artificially caused by a chemical carcinogen, was the lowest *. In rats, the incidence of breast cancer increased rapidly with an increase in the proportion of fat in the total dietary energy intake from 15% to 30%, and a plateau in incidence was observed at the level of 30%E *.
An analysis of hundreds of experiments on various diets shows that higher intakes of both calories and fat independently increase the incidence of breast cancer in rats and mice *. The only question is how adequately the results of studies obtained on laboratory rodents can be projected onto humans *.
What about primates? Female monkeys consume an average of 7% of their energy from fat (0.5-19.0%) *. In Paleolithic man, total fats provided more than 20% of the calorie content of food * *, of which saturated fats accounted for a third *. Note, however, that firstly, all fats that came with food were hidden, i.e. were part of food, and were not a refined food additive, similar to how we use oils now; and secondly, the ratio of fat intake was healthier.
An empirically reconstructed Late Paleolithic human diet would have provided ~3'000 kcal/day. At the same time, the average daily protein intake was 250 g (animal:vegetable protein ratio 2:1), fat intake – 70 g (animal:vegetable fat ratio 1:1.3), carbohydrate intake – 340 g, fiber – 46 g, calcium – 1'600 mg, vitamin C – 400 mg, cholesterol – 600 mg, and the ratio of potassium: sodium – 16:1 *. However, these figures strongly depended on the season and region of habitat *. Despite the fact that people usually did not experience chronic hunger, they had to make significant physical efforts to obtain and process food.
Reconstruction of the putative diet of East African Paleolithic humans has estimated the contribution of fats to total calories at 30-39%. The share of saturated fats here was only a third (11.4-12%), and the rest was accounted for by unsaturated fats – MUFA (5.6-18%) and PUFA (8.6-15.2%). The latter were high in α-linolenic acid (ALA), low in linoleic acid (LA) and high in long chain PUFAs. The average ω-3:ω-6 ratio was (0.8-1.9):1, and the average animal:plant food energy ratio was ~1:1. Due to the rich variety of sources used, nutrient intake was excellent *.
A review of the diets of modern hunter-gatherers of the equatorial zone (Kitawa, Trobriand Islands, Papua New Guinea) notes that in adults of these tribes, consumed fats provide only 20% of daily calories *. Elsewhere on the planet, the proportion of fat in the total caloric content of the diet of modern hunter-gatherers is 19-28% in Africa, and up to 58% in Alaska * *. Part of carbohydrates, depending on the geographical latitude, ranges from 15% to 50% *, and proteins – from 19% to 35% *. The ratio of energy animal:vegetable food ranges from 2:1 to 1:2 *. In any case, most of them are characterized by a high intake of fiber, antioxidants, vitamins and phytonutrients, a balanced ω-3:ω-6 ratio, and a low intake of table salt *. Thus, their «wild» diet is healthier and more complete than the modern «civilized» diet.
The diet of the Inuit (indigenous people of the Far North of America) requires more detailed consideration, since it is often, and quite erroneously, cited as a positive example of a high-fat diet.
A modeled traditional diet of nomadic Inuit, at an average calorie content of ~ 3'000 kcal, provides ~ 50% energy from animal fat, ~ 30-35% animal protein, and < 15-20% carbohydrate, primarily as liver glycogen *. Seal meat is the most commonly consumed, followed by fish, game birds, whale meat, and land animals *. From 1% to 4%, but not more than 10% of their food is of vegetable origin *. The marine fat they consume is rich in beneficial ω-3 fatty acids such as EPA and DHA, and their meat is rich in heme iron *. Despite the rather high calorie content of this model, the Inuit in past centuries experienced long periods of low-calorie nutrition during the periods of the polar night, when game production became difficult.
Over the past six decades, the nomadic way of life of the indigenous inhabitants of the Far North of America has undergone significant changes. As time goes on, they are increasingly moving away from their traditional carnivorous diet. Today, ~ 80% of the population lives in an urban setting, with low levels of physical activity and high food intake typical of a «Western» diet.
Due to the addition of potatoes, refined flour and sugar to the diet, the proportion of fats in the total calorie content of Alaskans fell to the average European 38%, of which a third is saturated fat * *. With an average calorie content of 2'700 kcal, sugar (160 g/day) makes up half of all carbohydrates consumed, providing 24% of daily calories, and more than 40% of all energy from foods recommended for women *. At the same time, 92% of Inuit women still have insufficient intake of fiber, and more than half of calcium and vitamins D and E. Other Alaskan indigenous peoples (Indians, Aleuts) also adopted a similar dietary profile (~ 40%E from fat, 18%E protein; 42%E from carbohydrates), with an average daily caloric intake of up to 2'000 kcal *.
As we can see, the traditional Inuit diet, which can hardly be called healthy, but to which their body has been genetically adapted for thousands of years, is very quickly replaced by another diet rich in sugar, which turns out to be even worse. Unfortunately, we do not have enough reliable data to compare the health of Inuit who strictly follow their traditional diet with the health of Inuit who do not. For this reason, all arguments about the universal benefits of a high-fat diet look like speculation. We can only consider the current state of affairs, but it looks depressing.
Over the past 30 years, breast cancer rates in Alaska have increased by 31% *. Among the Alaska Native population, 135-145 cases of breast cancer per 100'000 people * * * *, are recorded annually, which is an unconditional world anti-record. This is 1.3 times worse than in Belgium, which has the worst incidence rates of any country in the world. Mortality from breast cancer among Alaska Native women is also significantly higher *, despite the fact that two-thirds of cases are diagnosed at an early stage.
Due to the extremely low fiber intake of Alaskan Indians (< 15 g/day *), their incidence of colon cancer is 2.5 times higher than that of New Mexico Indians *. The age-standardized rates of cancer of the lung, cervix, nasopharynx and salivary glands among the Inuit population are also among the highest in the world, as are the rates of cancer of the esophagus and kidneys in Inuit women *. Survival rates for patients with various types of cancer among Alaska Natives are the worst compared to other populations in this region * *. And the average life expectancy of modern Inuit (64-67 years) is 12-15 years less than that of the average Canadian.
Of course, it is impossible to argue that these associations are provided solely by a large amount of high-glycemic carbohydrates, a small amount of fiber and a poor quality of fat. However, the strong influence of these factors on the health of the Inuit is undeniable. In any case, even 30 years ago, the situation with the incidence of breast cancer was extremely unsatisfactory. The good health and longevity of the Inuit due to their high fat intake is just an urban legend that is not supported by the facts.
Interestingly, in Greek women, the incidence of breast cancer is 2-3 times lower than in Inuit women, despite the consumption of the same 38%E from fat and approximately the same daily caloric intake of 3'700 kcal. In contrast to the High North with its low fiber intake and high animal fat intake, Greece has a rather high intake of fiber and olive oil (~ 150 g/day).
Let's look at the composition of fats consumed by these two groups being compared. In animal fat, the content of SFA and PUFA is approximately equal, and MUFA in it is only 11%. Olive oil is mostly MUFA and has 5-6 times more PUFA than SFA. In addition, olive oil is high in phytonutrients, and the absolute and relative content of pro-inflammatory ω-6 fatty acids is one of the lowest among the most abundant vegetable oils *. As a result, the possible antitumor effect of fatty acids of unrefined olive oil is more than covered by the antitumor effect of all its other components *.
In other studies, MUFA was associated with an increased risk of breast cancer only when animal meat provided the bulk of the MUFA. When olive oil was the predominant source of MUFA, MUFA was associated with reduced cancer risk and mortality * * *. In a study of women in southern France, higher olive oil intake compared to lower olive oil intake also markedly reduced the risk of breast cancer *. A special systematic review and meta-analysis found that the highest category of olive oil consumption, compared to the lowest, was associated with a 2-fold reduction in the risk of any type of cancer; including breast cancer *.
In a meta-analysis, after adjusting for alcohol and tobacco use, the relative risk of cancer between the groups with the highest and lowest levels of olive oil consumption was 62%. And there was more than a 5-fold difference in risk between those who consumed mostly olive oil and those who consumed primarily butter * *. With this in mind, the huge difference in incidence between Inuit and Greek women becomes understandable. So if one were to argue in favor of a high-fat diet, then the example would be the diet of the inhabitants of Greece, but not Alaska.
Based on this, it can be assumed that even with a fairly high calorie diet, you can significantly reduce the risk of cancer if you increase your consumption of plant foods, and replace vegetable oils rich in omega-6 with olive oil.
Let us add to this that among the same Inuit, one can distinguish several different food patterns. Ceteris paribus, a diet high in fish (PUFA ω-3), high food diversity, and low sugar intake is associated with a lower prevalence of coronary heart disease (CHD), myocardial infarction (MI), stroke, and hyperlipidemia. And a diet high in animal fats and marine mammals (SFA) is associated with a higher prevalence of CHD and MI, even with a low intake of simple carbohydrates *.
So, high-calorie food, including those caused by fat intake, can be no less of a problem than simply choosing the wrong type of fat. Incidence and mortality from breast cancer in different countries are as strongly correlated with any particular type of fat (SFA, MUFA, PUFA) as with the total amount of dietary fat *.
This association has been found in a number of other prospective studies. The risk ratio for invasive breast cancer in postmenopausal women at 40% energy intake from fat compared to 20% intake was 32% higher *. And the relative risk of breast cancer in women with 30-35% energy intake from fat compared to 20% was 15% higher *. Each additional 77 g of fat per day increased the risk of breast cancer by 35% *. Conversely, a population-based, multi-ethnic study suggests that a low-fat diet may play a significant role in breast cancer prevention *.
Indeed, if we compare the top 10 breast cancer-prone countries with the top 10 worst-performing countries, the latter group has a 27% higher calorie intake, while fat intake is 67% higher. It looks like we can significantly reduce the risk of breast cancer just by minimizing fat intake, resulting in a drastic reduction in total calories.
The cell itself does not care what source of excess energy comes from – fats, proteins, carbohydrates or alcohols. In any case, this inclines it to reduce mitochondrial activity and increase glycolysis. Therefore, regardless of the balance between these nutrients, we should aim for as low a calorie intake as possible.
The results of observational studies show that with a significant reduction in the total calorie content of food, the amount of fat in it turns out to be a secondary problem * * * * *. The consumption of even exclusively fats with an overall low calorie intake does not cause negative consequences, while saturated fats with an excess of calorie intake can cause fatty liver and, apparently, many other negative results.
This leads to another important conclusion:
The problem of the amount of fat in the diet begins to manifest itself significantly only after exceeding a certain calorie threshold, close to the physiological minimum of calories.
This assumption is supported by a number of experiments on rodents with breast cancer initiated by a carcinogen. Cross-feeding manipulations of female rats showed that on diets without caloric restriction, tumor growth was observed at both low (25%E) and high (45%E) fat diets. At the same time, the 35% caloric restriction diet significantly inhibited tumor growth, especially at low fat levels *. In other words, if the animals do not limit the daily caloric intake, then only reducing the fat content in the diet does not provide a significant antitumor effect.
Another dietary study in rats found that a low-fat, high-calorie diet led to a greater incidence and recovery of breast tumors than a low-calorie, high-fat diet. Caloric restriction (even with a simultaneous increase in the proportion of fat in total calories) led to a complete suppression of the formation of mammary tumors caused by a chemical carcinogen *. In many other experiments, caloric restriction also reduced the incidence of cancer in rodents, regardless of the amount of fat in the diet * *. At the same time, a change in the amount of protein consumed (in the form of casein) did not affect the incidence .
With a 30% decrease in the level of caloric intake from the level of nutrition without restrictions, the development of the tumor process in experimental rats was noticeably inhibited (14-20%). Although the proportion of fat in the isocaloric diet was raised in various experimental subgroups from 25%E to 45%E due to carbohydrates, tumor development in them increased slightly (7-13%) *. A plateau in tumor incidence was observed at 35% energy from fat. In all cases, the tumor growth rate compared to the control group was lower in the calorie restricted subgroups. The fat composition did not significantly affect oncogenesis in a wide range of changes in the amount of PUFA (linoleic) and SFA.
Similar results were observed even with only a 12% reduction in caloric intake compared to ad libitum (due to reduced fat intake). In the ad libitum groups, rats fed a 20% corn oil diet had a significantly higher number and mass of mammary carcinomas compared to rats fed a 5% corn oil diet. When rats were calorie restricted, the number or weight of mammary tumors in the 20% corn oil group increased by only 12% compared to the 5% group *. That is, the fat factor becomes important with an increase in the caloric content of the diet.
In another cross-over experiment, a low-fat, high-calorie diet resulted in a higher incidence and yield of tumor than a low-calorie, high-fat diet. Caloric restriction (even with an increase in the relative proportion of fat intake) led to a strong suppression of the formation of tumors initiated by a chemical carcinogen *. This is another argument in favor of a low-calorie diet.
Even with a high fat diet, a 40% reduction in caloric intake has been shown in preclinical studies to restore control of glucose metabolism and improve blood pressure in obese and hypertensive animals * *. On a human equivalent basis, a 40% calorie cut is equivalent to a reduction in calories from 3'600 kcal/day to 2'200 kcal/day. Or, this can be equated to reducing calorie intake in countries with the highest incidence of breast cancer to the level of calories in countries with the lowest incidence (see graph †).
The results of experiments with specially genetically modified animals cannot always be correctly projected onto people. And manipulation clinical trials with such a design should not be expected. However, all of these preclinical results strongly suggest that in humans, high caloric intake may be as significant a carcinogenic factor as dietary fat itself.
Large multi-year studies show that reducing the contribution of fats to total caloric intake from 35% to 20%, combined with increasing consumption of fruits and vegetables to 5 servings per day and grains to 6 servings per day, even while maintaining a caloric intake, definitely reduces the risk of invasive disease. breast cancer in postmenopausal women * * *. A low-fat, high-carbohydrate diet for 2 years can reduce the area of mammographic breast density * *. And this is even without reducing the calorie content of the diet, which was significantly higher than the physiological minimum!
A large European study found that a diet high in saturated fat increased the risk of developing ER+ and PR+ breast cancer *, while high-fat dairy products contribute to the progression of localized prostate cancer *. Conversely, after diagnosis, a low-fat diet (≤ 20% of total calories from fat) significantly increased survival * and nearly halved breast cancer mortality compared with a regular diet (≥ 30% of total calories from fat) * * *.
A significant number of other studies conducted in European countries found no benefit from reducing fat intake and quickly declared no effect of fat on morbidity. However, a detailed analysis of the results shows that in these studies, the lower threshold for fat intake did not approach 20%E, which is clearly not enough to reveal the effect we are studying. The reduction in energy intake from fat from 40% to 33% is still a manipulation in the exorbitantly high areas of total caloric intake considered in these studies. Changing fat intake by 5%E on a high-fat diet has no significant effect, while reducing it below 20%E gives impressive results *.
A high-fat diet increases not only the risk of cancer, but also the risk of its metastasis. In animal experiments, it has increased the number and size of metastatic deposits in the lymph nodes *, and there is good reason to expect a similar effect in humans. In an intervention study in women with resected breast tumors at an early stage of cancer, reducing dietary fat intake from 51 g/day to 33 g/day (from 29.2%E to 20.3%E) while maintaining nutritional adequacy, on the contrary, was accompanied by a slight decrease in the relative risk of a 5-year recurrence of the disease (from 12.4% to 9.8%) *.
The US Institute of Medicine, in its 2002 guidelines, suggests consuming 20-35% of all energy from fat *. However, the array of evidence suggests that we are probably better off aiming for the lowest end of the proposed range. In addition to the risk of obesity, diabetes, cardiovascular disease, and cancer, highly oxidizable vegetable oils are suspected to be responsible for the accumulation of amyloid and tau proteins associated with Alzheimer's disease *.
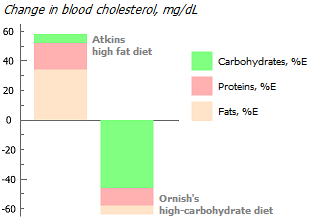
Comparative analysis of various popular diets shows that within a month, the Atkins diet, rich in fat and poor in fiber, raises the level of cholesterol in the blood serum, thereby increasing the risk of cardiovascular disease. At the same time, Ornish's high-fiber, low-fat diet, on the other hand, lowers cholesterol * *.
A low-carb, high-fat diet has also been noted to increase markers of inflammation * *. While a high-fiber, low-fat diet reduces them *, which will be beneficial in any clinical setting.
In conclusion, let us once again draw attention to the fact that we cannot talk about the health effects of a high- or low-fat diet without distinguishing between the classes of fatty acids. Ruminants are herbivores, but in fact their main source of energy from food is short-chain fatty acids, which are produced in the intestines of animals from the fiber they eat. Thus, they are actually fat-eating animals rather than herb-eating animals.
The same can be said for vegans, who show a significantly lower risk of mortality from the leading causes of death. The invisible and often ignored production of short-chain fats within the body has extremely beneficial effects on human health. In contrast, dietary intake of long-chain fatty acids, as discussed above, has adverse health effects.
The biological reason for the negative impact of fatty acids on cancer development has long been a mystery. But recently, this mystery is beginning to be unraveled. At least when it comes to the effect of fat on metastasis. Researchers have identified cells that are unique in their ability to initiate metastasis. These cells express high levels of a fat receptor (CD36), known as the «fat controller» *. Thus, a diet high in fat, especially palmitic acid, increases their metastatic potential *. Conversely, blocking the cellular receptor CD36 causes almost complete suppression of metastasis in experimental mice.
In laboratory conditions, blocking the CD36 receptor suppressed metastasis in breast *, brain *, ovarian * and prostate * cancer. Importantly, inhibiting CD36 weakens the migration and invasion of breast cancer cells regardless of the subtype of breast cancer *. Thus, CD36 inhibitors look promising in the fight against metastasis. However, limiting dietary fat intake rather than using CD36 receptor inhibitors seems more reasonable. It is time to abandon the established dogma that simple sugars are the only promoters of cancer. Lipid metabolism plays no less a role *.
Conclusions. General recommendations can be reduced to limiting the intake of total fats to 15-20%E if the caloric intake exceeds the physiological minimum (for women of an average configuration, this is 1'600 kcal/day). And if we consider the varieties of fats, then to the rejection of the use of vegetable fats rich in ω-6 fatty acids (sunflower, corn, soy, rapeseed, safflower), limiting long-chain saturated fatty acids (animal fat), expanding the use of medium-chain fats (coconut, seafood, nuts) and a total elimination of trans fats. And besides, to an increase in the production of short-chain fatty acids from plant fiber by intestinal bacteria.
Modification of dietary fat intake should increase the following ratios:
- unsaturated fats : saturated fats;
- monounsaturated fats of vegetable origin : monounsaturated fats of animal origin;
- fatty acids ω-3 : ω-6;
- short and medium chain fats : long chain fats;
- fiber : total fats *.
The ratio of different classes and subclasses of fatty acids can be improved, for example, by replacing red meat with fatty ocean fish. Despite the ever-increasing danger of getting toxic metals flooding the ocean with fish, the benefits of it outweigh the disadvantages; at least during the period of growth and maturation of a woman *. In contrast, eliminating fish from the diet is associated with a significant increase in the relative risk of breast cancer *.
The consumption of animal fats in countries with a low risk of cancer is at least twice as low as the consumption of vegetable fats. In addition, in these countries, for the most part, fats are consumed hidden in food products (in meat, nuts, oilseeds), and not in the form of a separate food component (vegetable oil).
Of course, it is not easy to reduce the consumption of fatty foods in conditions when the feedstock itself is saturated with fat. But we are quite capable of reducing our dietary fat intake by cutting out vegetable oils (especially those rich in ω-6), fatty meats and lard, and industrially processed foods that are rich in added fat, especially trans fats. It is worth recognizing that, according to calculations, even with the complete rejection of fat supplements in food, it is very problematic to reduce the contribution of fat to total calories below 20% using the food products offered by the modern market. Therefore, reducing the total calorie content of the diet seems to be a more reliable solution to the problem.
Protein. The median protein requirement of a healthy adult population is 0.65 g per kg body weight per day, and the recommended daily intake (97.5th percentile) is 0.83 g/kg per day *. Thus, the recommended protein intake for a person weighing 60 kg will be about 50 g/day *, which corresponds to ~ 100 g of lean meat per day. In this case, with a daily calorie content of 1'600 kilocalories, the contribution of protein to the total calorie content will be 15%. However, it can be increased up to 20%E for people over 65 when they start to lose muscle mass.
As with fats, the source of dietary protein is very important.
Protein is divided into vegetable and animal. Plant and animal sources of protein differ in the amount and ratio of amino acids in their composition. Animal protein, in comparison with vegetable protein, is much closer to human protein in its amino acid composition. It contains all essential amino acids; for this reason, it is considered to be more complete. However, this does not mean that it is more useful.
Meat and organ meats are high-calorie foods that are much poorer in nutrients than vegetables, especially dark green leafy vegetables. Animal protein is rich in amino acids such as methionine, asparagine and arginine, the restriction of which reduces the ability of the tumor to grow and metastasize * *. Replacing animal protein with vegetable protein can slow down the production of new cells. While this may not be desirable in bodybuilding and wound healing, it is good for cancer.
In general, animal protein, precisely because it is a «high quality» protein, i.e. rich in essential amino acids, will stimulate the activity of insulin-like growth factor (IGF-1) and thus promote cell division; while «low quality» vegetable protein will generally have the opposite effect *.
Plant and animal sources of protein also differ in the content of carcinogenic toxins. The flesh of animals accumulates in itself many hard-to-remove carcinogenic toxins coming from food. For example, if it takes about 7 kg of grain to produce 1 kg of meat, then from 1 kg of meat we can take in about the same amount of pesticides or heavy metals as from 7 kg of grain. Thus, replacing animal protein with vegetable protein can reduce food toxicity by several times.
There are other dangers from commercial meat besides toxins and cell growth-stimulating amino acids. The industrial production of meat requires the introduction of many undesirable substances into animals that are difficult to remove or neutralize during the cooking process. This means that along with meat, growth hormones, antibiotics and tranquilizers can enter the human body.
In addition, farm beef can be a source of pathogens, spongiform encephalopathy and bovine leukemia. Not everyone knows that heat treatment does not guarantee complete disinfection of meat raw materials. For example, tumor viruses such as polyomaviruses are able to withstand the temperature of food processing and then enter the body, disrupting mitochondrial function, damaging DNA and causing them to mutate *. To give the meat a presentation and to sharpen the taste, nitrites are often added to it, which, after combining with amines, form the strongest carcinogen – nitrosamine.
Meat can also contain or cause an increase in body levels of many other unwanted or dangerous chemicals such as TMAO (trimethylamine N-oxide), heme iron, heterocyclic amines, N-acetylneuraminic acid (Neu5Ac), etc. It is not known which of them is the most dangerous. However, it is obvious that each of them makes a small contribution, eventually summing up to a noticeable amount.
We can compare the nutritional value of 100 grams of different types of cooked meat using the table here (%DV – Percent Daily Value for Adults). Although the values given here are very approximate, they provide a clear demonstration of the benefits of one meat source over another.
According to the source of origin, the meat is divided into white (chicken, turkey, rabbit) and red (beef, pork, lamb). And according to the processing method, it is divided into unprocessed (boiled, stewed, baked in its own juice) and processed (sausages, bacons, smoked meats), which usually use smoking, nitrites and other pathogenic chemical compounds.
Different animal sources of meat, as well as the way it is processed, can have different, often opposite, health effects.
Consumption of red and processed meat is associated with modest increases in overall mortality, cancer mortality, and cardiovascular disease mortality *. The consumption of processed meat, compared with the rejection of it, can increase the risk of coronary heart disease by 18%, the consumption of whole meat by 9%, while the consumption of poultry does not affect this risk. What's more, consumption of white meat as part of a diet rich in vegetables has been associated with a reduced risk of obesity, cardiovascular disease, type II diabetes, and even cancer * * *. However, with increasing fat content of white meat and the degree of its processing, the risk increases, and the blood lipid profile worsens.
Milk is a liquid analogue of animal protein. Milk is often recommended as a natural and healthy product that contains high biological value protein, calcium, phosphorus, magnesium, potassium, zinc, selenium, vitamin A, riboflavin and vitamin B12.
Despite these benefits, milk poses a number of additional health risks. For example, there are significantly more growth hormones in cow's milk than in human milk, and incomparably more than in meat. Growth hormones stimulate cells to divide, which increases the risk of any type of cancer. In addition, milk increases estrogen concentrations. Consumption of 1 liter of cow's milk for an hour increases the level of estradiol in men by 1.8 times, estrone by 1.5 times and estriol by 3.7 times. And women's consumption of 0.5 liters of milk led to an increase in estradiol levels by 4 times, estrone by 3.7 times, and estriol by 3.8 times *. Another danger of dairy products is milk fat, which is rich in saturated fats. The fatter the dairy product, and the more often it is consumed, the higher the risk of breast cancer *.
In the wild, milk is not a natural adult food. Milk consumption by mammals (including primates) is limited to a short period of time after birth, when accelerated body growth and hardening of the infant's soft bones are required. With age, the ability to digest lactose in mammals is naturally lost. Man acquired genetic changes to maintain this ability relatively recently, in the Bronze Age, and it is not common everywhere. During the Paleolithic, when mammals were not yet domesticated, the consumption of dairy products by adults was practically zero.
In addition to dietary, infectious danger also comes from milk and meat. Thermally unprocessed cow's milk may contain bovine leukemia virus (BLV), which belongs to the Retroviridare family, like the human immunodeficiency virus. Although many European countries have reported the absence of BLV, the virus is widespread in many other countries around the world *. In the US alone, about 38% of beef herds, 84% of all dairy herds, and 100% of large dairy herds are infected * *. Not surprisingly, three-quarters of the Americans surveyed had antibodies to this virus *.
BLV is known to be able to transmit from animals to humans * *, and is strongly associated with breast cancer *. BLV viral DNA was found in breast tissue in 38% of women studied in the USA *. Although the virus is rendered harmless by high temperatures, there is a high risk that the virus can enter the body through insufficiently processed milk or meat.
In a prospective study of women in Southern France, the adjusted relative risk of breast cancer increased linearly by 57% when dairy consumption increased from < 134 g/day to ≥ 271 g/day *. However, the biological effects of different dairy products can be exactly the opposite due to different amounts of nutrients, biologically active compounds and microorganisms. While whole milk can increase cancer risk *, low-fat dairy products such as yogurt may have the opposite effect due to their «good» bacteria, calcium, and vitamin D.
A large-scale prospective 14-year study of the association between dairy consumption and the risk of death from all causes, in which more than 100,000 people took part, came to similar conclusions. Frequent consumption of unfermented milk (≥ 2.5 times per day) increased the risk of all-cause mortality by 32% compared with infrequent consumption ≤ 1 time per week. The relative risk was directly related to the fat content of milk. At the same time, consumption of fermented milk products reduced the risk of total mortality by 10% *.
Thus, the benefits provided by fermented milk products to the large intestine may offset other harm from them. But this was a comparison between consuming fermented and unfermented milk, not between consuming milk and not consuming milk. Therefore, this observation rather speaks to the importance of lactic acid bacteria, which can be taken in the form of supplements, than to the benefits of dairy products in principle.
However, the main disadvantage of any dairy products remains – they contain too much calcium and little magnesium. Large amounts of calcium are required only for skeletal formation in newborn mammals, but in adult humans this can cause severe calcium:magnesium imbalance.
Eggs can also increase the risk of breast cancer * *. However, this association is observed with consumption of eggs above 5 eggs, and below 1 egg per week, while 2 eggs/week is an acceptable consumption level * *. A further increase in consumption is already beginning to have a negative effect *. However, similar conclusions were made based on data from countries with high calorie consumption.
The method of feeding the birds that produce the eggs is essential. The method of feeding the birds that produce eggs is essential. Eggs from free-range birds have a ω-3:ω-6 ratio of approximately 1:1.3, while eggs from grain-fed birds have a much worse ω-3:ω-6 ratio of approximately 1:20 .
Fish appears to be a better source of animal protein than meat, as polar fish oil has a significant advantage over animal fat. However, due to the pollution of the oceans, ocean fish, just like animal meat, are subject to the accumulation of toxins. From this point of view, the lower in the food chain an organism is, the safer it is. Therefore, seafood such as shellfish, shrimp, krill and small fish are preferred over tuna or squid.
The difference between wild fish meat and farmed fish meat is exactly the same as the difference between wild animal meat and farmed meat. First of all, this refers to the ratio ω-3:ω-6, as well as the saturation of meat with microelements.
Plants are lower in the food chain than animals. Therefore, the consumption of vegetable protein is several times less polluting the body with toxic metals and carcinogenic organic pollutants * than the consumption of animal protein. However, more important than this is the difference in the amino acid composition of animal and vegetable proteins.
As can be seen from the graph presented here, with an increase in the proportion of total protein in the calorie content of food, the incidence of breast cancer in women increases slightly. However, when comparing this with the other association of morbidity and total caloric intake †, it can be seen that the increase in protein intake coincides with the increase in total calorie intake. Given this factor, the effect of protein on morbidity can be drastically reduced. At the same time, the persuasiveness of the association between protein intake and cancer risk will decrease.
Although the current recommendation is 15%E as protein, we see that the real cancer risk reduction begins when protein intake is reduced to 9-12%E. However, as we know, the increase in human protein intake is mainly due to an increase in animal protein. Thus, the graph reflects the influence of predominantly commercial meat, i.e. animal protein with a high fat content. This means that some of the overall damage to meat may be due to the saturated fat† present in the meat, the heme iron, and the way the meat is cooked, and not just the protein itself. When replacing animal protein with vegetable protein, increasing protein intake may be safe.
Let's try to compare the influence of animal and vegetable protein. A meta-analysis of retrospective studies found that higher total protein intake was associated with higher all-cause mortality. However, animal protein turned out to be the only negative factor, because the consumption of vegetable protein, on the contrary, was associated with a decrease in both mortality from all causes * * * * * * and the risk of breast cancer * * *. Of all animal protein sources, processed meats were the most dangerous * and marine fish the least *.
A large-scale study of more than 81'000 people found that the group with the highest intake of protein from animal sources, compared with the group with the lowest intake, had a 61% higher risk of dying from cardiovascular disease. And the group with the highest intake of protein from plant sources compared to the group with the lowest intake had a 40% lower risk of death *. Replacing processed meats with a combination of poultry, eggs, fish, legumes, nuts, and low-fat dairy products reduces the risk of overall, cardiovascular, and respiratory mortality *.
In one prospective study, high vegetable protein intake was also inversely associated with all-cause and cardiovascular mortality *. An association has also been found between benign uterine tumors and a high intake of red/processed meats with a low intake of marine fish, green vegetables and fruits *. Finally, a systematic review found that for the same calorie intake, a higher percentage of calories from animal protein or a lower percentage of protein from plant sources are associated with an increased risk of overall mortality *.
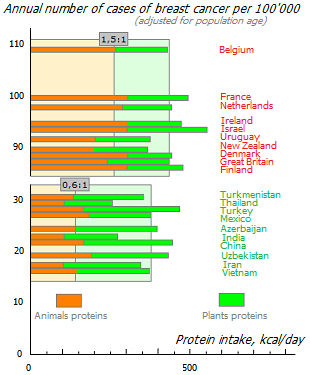
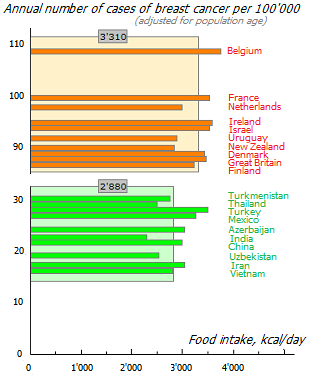
From the histograms shown here, it can be seen that the ratio of animal:vegetable proteins is 2.5 times higher (1.5:0.6) in the ten most disadvantaged countries in terms of the incidence of breast cancer compared to the ten most prosperous. And this is with approximately the same intake of total protein * and only a 15% difference in total calories. In a similar histogram, already estimating the ratio of animal:vegetable fats †, the difference between the prosperous and disadvantaged dozens of countries differed by half.
This was a comparison of countries where the predominant type of cancer is breast cancer. If we compare the top ten countries with the best rates of all types of cancer, we can see that their consumption of meat and animal fats is even lower, with almost equal consumption of all other food categories †.
It can be argued that observational studies have weak evidence due to the presence of a large number of concomitant factors. For example, a person's high consumption of processed meat is often associated with low physical activity, high fat and alcohol intake, and generally poor health care. However, the positive role of reducing animal protein intake is supported by manipulative studies *.
Replacing animal protein in the diet with soy protein slowed the development of lung cancer in experimental mice *. In addition, in mice on an unrestricted diet, replacing carbohydrates with an equivalent amount of vegetable protein in calories resulted in slower growth of the grafted tumor *. Animals on a diet containing 20% of total calories as vegetable protein had 37% slower growth in grafted tumor weight relative to animals on a diet containing 20% of total calories as animal milk protein *.
On a low-protein diet (10% of total calories as protein), it no longer mattered for the rate of tumor growth in animals whether the protein came from a vegetable or an animal source. Of course, the results of animal studies are not necessarily applicable to humans. However, the amount of protein consumed remains an important factor for humans as well.
Reducing the ratio of animal to vegetable proteins in the diet significantly delays the development of prostate cancer in men *. Similar associations can be expected for breast cancer, because in regions with a low incidence of breast cancer, the ratio of vegetable:animal protein in food varies between 3:1-2:1, and in regions with a high incidence, the ratio is reversed – 1:1.2-1.3 *.
In a systematic review fully adjusted for total calorie, alcohol and fiber intake, age, sex, smoking, and BMI, there was an increased risk of total mortality when carbohydrates or unsaturated fats were replaced with animal protein while maintaining total caloric intake *.
Studies of the long-term effects of calorie and protein restriction have shown that short-term (6-10 days) fasting or protein restriction reduces serum concentrations of the potent proliferation stimulator insulin-like growth factor (IGF-1). However, even long-term severe calorie restriction is unable to reduce IGF-1 if protein intake remains high *. Compared to the control group («Western diet»), the decrease in IGF-1, CRP and insulin levels was 2-3 times lower in both the «low-calorie» diet group and the «low-protein» diet group. However, the decrease in IGF-1 levels and the IGF-1:IGFBP-3 ratio was greater with the low-protein diet, and the decrease in insulin and CRP was greater with the low-calorie diet.
In general, the sum of the knowledge accumulated to date gives some reason to believe that increasing the proportion of protein in the diet may be less dangerous than increasing the proportion of saturated fat. And that the quality of the protein (origin, fat content, ecological cleanliness, the principle of animal feeding, etc.) is more important than its quantity *. Results from a manipulative comparison of low-calorie diets (-30%E) indicate that the type of protein consumed affects systemic inflammation status much more than the total amount of protein consumed. Animal protein from animal meat was associated with increased levels of inflammatory markers, while plant protein and protein from marine fish were not *.
The specific protein intake of higher primates living in the wild is about 2-3 times higher than the norm recommended for humans *. Female chimpanzees can consume between 4% and 33% of food energy in the form of protein *. But with the availability of any food, they maintain a total protein intake of ~ 12%E *. The main source of protein in primates is of plant origin.
In the diet of Paleolithic humans, animal food sources provided about a third of all calories consumed * *, which is twice the current recommended amount. A study of the diets of over 229 different ethnic groups of modern hunter-gatherers shows that animal protein provides between 19% and 56% of their total calories *. However, the quality of this meat is much higher than that which the food market offers us *.
The flesh of wild animals usually differs markedly from the flesh of farm animals in the amount of fat (respectively, 2-4% vs. their low quantity, the absence of pesticides and other toxins against their presence). Only by autumn does the fat reserve of wild animals increase; especially in large animals, and especially in arctic regions. Herbivores build up their weight by consuming the natural resources intended for them by nature – plants.
At the same time, farm meat is obtained using technologies for rapidly increasing the mass of animals, and the animals themselves are in conditions of life and nutrition that are far from natural. In fact, the increase in meat consumption by hunter-gatherers means an increase in the consumption, for the most part, of protein. And the increase in the consumer's consumption of store-bought meat also means an increase in the consumption of saturated fat and harmful additives used in the process of raising animals.
Let us once again note that almost all of the clinical and observational studies mentioned above have studied the effect of consumption of farm meat, including processed meat, rather than game. This may be another reason why, in the same studies, a high intake of plant protein did not pose a risk, while a high intake of animal protein did.
Pro-inflammatory markers rise within a few hours of eating fatty meats (domestic beef), but not after eating lean meats (kangaroo) *. Obviously, the consumption of wild-raised game is not as dangerous as the increase in the consumption of farmed meat. However, fatty meat even from wild animals will not be the best choice of protein food. The largest amount of oily game is found in the diet of the Alaskan Natives (Inuit), who follow the traditional semi-nomadic hunter-gatherer lifestyle. At the same time, they cannot boast of good health and longevity, but rather, on the contrary *. For example, the incidence of breast cancer in the Inuit population is probably the highest on the planet *.
There are plenty of compelling reasons to change the quality of your protein intake. For example, to shift the focus from red meat to white. And also to switch from meat of domestic animals to the meat of marine life and, in general, from animal protein to vegetable protein *. Unlike hunter-gatherers, who eat only what they can get for their day, modern humans have the ability to determine their own diet.
Although Homo sapiens evolved with a high consumption of animal protein, the older vegetarian way of eating may still fit our genotype better than carnivory. Based on this belief, or for some other reason, some people turn to veganism. The benefits of veganism are still more of a matter of faith than undeniably proven scientific fact.
Renowned vegan advocate Dr. Michael Greger* provides numerous, varied and compelling evidence for the benefits of this style of eating *. However, nutritionists are still not convinced that cutting out animal protein is better than limiting it *. No evolutionary stage of human development and no country in the world gives us an example of a true vegan diet.
However, this style of eating is perfectly acceptable. The Academy of Nutrition and Dietetics is of the opinion that in the case of a vegetarian diet, a variety of plant foods can provide adequate amounts of essential amino acids and essential fatty acids at a physiological calorie intake *.
The results of retrospective studies show that, despite some concerns *, even a long-term vegan diet (low-fat, plant-based whole food) does not cause a lack of protein, iron, calcium and essential fatty acids *. Consuming protein exclusively from plant sources can also provide the body with all the necessary amino acids * *. Although animal protein is considered more complete than plant protein, this is not always the case. Examples of complete plant protein sources include hemp seed, chia, quinoa, and soy.
At the same time, veganism can create some domestic inconveniences. When switching to a vegan diet, you will have to monitor the intake of zinc, iron, iodine, taurine, EPA and DHA, as well as vitamins B6, B12 and D, because. with a complete rejection of meat, their deficiency is possible *.
It is interesting to look at the results of dietary experiments on animals. One of them compared the health outcomes of mice fed on 25 diets with different ratios of carbohydrates (starch and sucrose), proteins (casein and methionine), and fats (soybean oil). As the carbohydrate:protein ratio increased, the median health and longevity scores of mice increased *. Brain aging in rodents was also somewhat inhibited on a low-protein, high-carbohydrate diet *.
Amino acids, especially branched chain amino acids (BCAAs), are key signals for insulin release and mTOR activation * * – key factors in health and aging * *. As the carbohydrate:protein ratio in the rodent diet decreased, BCAA levels continuously increased, reaching a plateau at about 1.5:1. Although insulin levels were affected by both dietary protein and carbohydrates, they were minimal when protein intake was lowest *. The latter fact may explain the observation that high protein and cholesterol intake is associated with the development of glucose intolerance * *.
In another experiment, reducing animal protein intake from 21% to 7% of total calories (to the lowest possible level) reduced the growth rate of grafted breast cancer in animals. Variation within the same limits of consumption of plant proteins did not affect the development of the tumor – both at their maximum and minimum consumption, the tumor grew at the same rate as with a low consumption of animal protein *.
Overall, animal eating patterns without calorie restriction, but with a low protein:carbohydrate ratio, have been associated with lower blood pressure, better glucose tolerance, higher HDL levels, higher mitochondrial activity, and a significant delay in the aging process *. These results are in good agreement with observational studies in which long-term diets with a high protein:carbohydrate ratio are associated in humans with increased incidence of cardiovascular disease * *. More than 10% of dietary calories from protein are associated with an increased risk of diabetes, cancer, and all-cause mortality *. In passing, we note that regardless of seasonal changes in their diet, free-choice female chimpanzees, like other carnivorous primates, try to maintain protein intake (including plant sources) at ~14%E *.
People aged 50-65 years who followed a high-protein diet throughout their lives had a 75% increase in overall mortality over the next 18 years, and a 4-fold increase in the risk of dying from cancer *. The researchers noted that a high-protein diet in this case means a diet with a significant amount of animal protein – such is the structure of the diet of modern man.
Low protein:carbohydrate diets without calorie restriction are thought to be associated with increased body fat with decreased lean body mass, as well as fatty liver disease. However, when considering a high-carbohydrate diet, one should pay attention to the ratio of simple and complex carbohydrates in it. The accumulation of body fat is associated with simple, not complex carbohydrates *.
It is also worth noting that in old age the effect of protein decreases or even reverses *. Thus, low protein intake may be beneficial in young adulthood, but not later in life *.
Indeed, a diet high in (> 20%E) animal protein (red meat, poultry, fish, dairy, and eggs) compared to a diet low in protein (< 10%E) is associated with an increased overall risk of cancer mortality by more than than 3 times in persons younger than 65 years. True, these associations were either weakened or canceled if the source of the protein was vegetable. At the same time, in people over 65 years of age, high protein intake was associated with reduced cancer risk and overall mortality, but with a 5-fold increase in diabetes mortality across all age groups *.
In older adults, increasing protein intake is commonly recommended for sarcopenia as a way to combat muscle loss and bone loss. Again, plant-based rather than animal-based protein is preferred. A specific clinical study found that protein intakes above the recommended daily allowance (0.8 g/kg body weight) did not increase lean body mass in older men *, but the source of the protein was not specified in the study report.
At the same time, it is worth recalling that inadequate functioning of the gastrointestinal tract can make a significant contribution to the adverse effects of protein intake.With age, the ability of the stomach to secrete acid and the ability of the pancreas to secrete proteolytic enzymes usually decrease. Both the first and the second worsen the breakdown of protein into amino acids. Insufficiently digested protein, entering the large intestine, is used as food by those types of intestinal bacteria that are classified as pathogenic bacteria, and will help them flourish.
In addition, the incompletely digested animal protein is recognized by immune cells as an infection, which exacerbates the inflammatory state. Increasing protein intake under such conditions may have adverse effects. To avoid them, elderly people or those with insufficient enzyme production can, on the recommendation of their doctor, take appropriate supplements (hydrochloric acid and/or proteolytic enzymes) along with protein.
As evidence of the benefits of a low-protein diet, the example of Okinawans is often cited, which has the highest specific number of centenarians and a very low incidence of all types of cancer. The amount of carbohydrates consumed by the centenarians of Okinawa in the previous years of their lives was 85% of total calories, and protein – 9%, with most of the protein coming from plant sources *.
However, in this case we are also dealing with a low-calorie diet at a younger age (caused by the war), and this may be as significant a factor in reducing cancer risk as a low protein diet *. For example, an 80% reduction in protein intake (from 20%E to 4%E) increased the average lifespan of rodents by about 15%, while a 40%E reduction in calories increased it by as much as 30% *.
On average, for the top five countries with the lowest overall incidence of all types of cancer (Gambia, Yemen, Niger, Tajikistan, India *) weekly consumption of meat does not exceed 250 g, fish – 140 g, dairy products – the equivalent of 1 liter of raw milk, and eggs – 10 g (i.e. less than 1 egg per month). In the Gambia, for example, protein provides only about 15% of all dietary calories *. This level of protein intake is close to that offered to adult women by the US Institute of Medicine – 46 g/day *.
The general recommendation for proteins is to limit their intake to less than 15% of total calories, with no more than one-third of this amount from animal origin. Increasing protein intake above this value is possible, provided that it is vegetable protein.
The best sources of vegetable protein are legumes and nuts; and animal protein – game, poultry, rabbit and fish of the polar seas.
Carbohydrates are the main raw material for the energy supply of body cells. For the production of ATP, glucose is primarily used, and after its depletion, liver glycogen. If this is not enough, fat is used as an energy source. When the intake of external sources is insufficient, the protein structures of the organism itself begin to be metabolized, starting with the most unnecessary ones.
There are three main classes of dietary carbohydrates:
1) simple carbohydrates (mono- and disaccharides) – respectively, individual saccharide molecules (glucose, fructose, galactose, sucrose) or short chains of two saccharide molecules that quickly enter the blood from food without prior fermentation;
2) complex carbohydrates (polysaccharides) such as starch – longer chains of carbohydrate molecules (three or more) that require prior enzymatic breakdown in the digestive system before entering the bloodstream;
3) fiber – complex carbohydrates that are not cleaved by the enzymes of the body due to the lack of such in humans; and which are broken down by enzymes found in certain types of intestinal bacteria.
All of them are eventually broken down into glucose before they enter the cell as food. However, dietary intake of various classes of carbohydrates causes a rise in blood glucose concentration in different ways, because each of them has its own rate of breakdown to glucose.
Metrics such as the glycemic index (GI) and glycemic load (GL) * are used to assess the ability of a food to raise blood glucose levels. The GI evaluates the rate at which blood glucose levels rise after eating a particular food, while the GL evaluates the quantity and quality of carbohydrates in a serving of food.
The figure below shows an example of how two different classes of carbohydrates, with an equal amount of glucose formed from them (area under the curve), form curves with significantly different blood glucose saturation amplitudes.
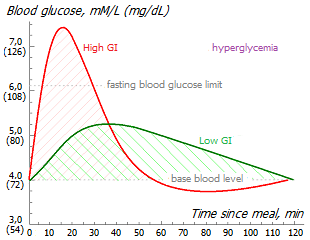
Simple carbohydrates (mono- and bisaccharides), compared to complex carbohydrates, have a higher glycemic index. Those. they are absorbed very quickly or metabolized quickly, creating a high concentration of glucose in the blood. To bring glucose back to normal, the pancreas releases insulin into the blood, which enhances the transfer of excess glucose to the cells of the body. Weakness, fatigue of the body or brain, drowsiness, «blurred» thinking after eating are common symptoms of a spike in blood glucose/insulin.
Excessive glucose, like excessive insulin, negatively affects breast health. A meta-analysis shows that a chronic rise in blood glucose levels greater than 6.1 mM/L increases the risk of all cancers by a third *.
Insulin increases the level of latent systemic inflammation, which naturally accelerates the degenerative processes in the body, which are accompanied by chronic fatigue syndrome, aging, Alzheimer's disease and cancer of any origin. In particular, insulin stimulates the division of mammary epithelial cells * and the insulin receptor is overexpressed in breast tissue *.
By reducing your calorie intake, we can reduce the production of free radicals. Thus, minimal harm to glucose should be expected when calorie intake is not higher than the physiological minimum. For women of average build and moderate physical exertion, this is approximately 1'600 kcal/day.
The safe level of glucose in the blood is not exactly defined. It is generally accepted that this is 5.6 mM/L (100 mg/dL) on an empty stomach, and 7.8 mM/L (140 mg/dL) 2 hours after a meal *. However, these figures may actually be too high.
Since 1980, the prevalence of type 2 diabetes among adults worldwide has quadrupled *. About 11% of American adults have diabetes and another 27% are pre-diabetic *. One in five American teenagers suffers from diabetes or pre-diabetes *, and the number is rising alarmingly. In other «wealthy» countries, a similar situation is observed. If we consider the change in dietary patterns in the United States since 1961, it is easy to see that during this time there has been a significant increase in the consumption of grains, sugars, and especially fats, which account for the bulk of the increase in total caloric intake *.
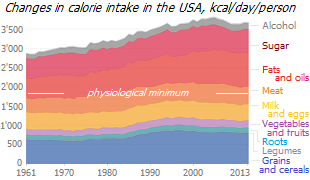
In parallel with the explosive growth in the incidence of diabetes, there is an increase in the incidence of other degenerative diseases. And a significant contribution to this trend is made by the growing consumption of sugar from year to year. Unfortunately, nutritionists are not yet ready to offer a total sugar-free diet, and the general public is not yet ready to accept such a proposal.
The US Dietary Guidelines suggest reducing the amount of added sugar in your diet to 10% of your total calories *, but even that amount of sugar looks grossly overpriced. The food of ancient hunter-gatherers was not rich in simple carbohydrates – fruits were wild, i.e. were low in sugar and high in fiber, and honey was a rare delicacy. Even just a mere 150 years ago, there was little to no extra sugar in the diet, and diabetes showed no signs of an epidemic.
The impact of simple monosaccharides and disaccharides on cancer risk is not limited to the glycemic effect alone. As with fats, the formula for simple sugars also matters. Different monosaccharides and disaccharides may affect breast cancer risk in different ways through various, as yet poorly understood, mechanisms.
The type of carbohydrates and their digestibility largely determine the physiological responses in relation to protein and nutrient metabolism in the liver, as well as in relation to the intestinal microflora. A comparison of 33 isocaloric diets in animal studies showed that diets low in protein (10%) and high in carbohydrates (70%) promote the healthiest metabolism when carbohydrates are high in non-fermentable polysaccharides. And the worst results were at the ratio of monosaccharides fructose:glucose ~ 50:50 *, i.e. at the ratio observed in ordinary food sugar.
Thus, even different simple carbohydrates have different effects on our health. Consider, as an example, the question of why an increase in fructose intake creates a risk of disease, but an increase in glucose intake does not.
The metabolism of glucose and fructose differs significantly *. Glucose from food is converted to pyruvate by the enzymes hexokinase (glucokinase) and phosphofructokinase. The activity of these enzymes is limited when the concentration of pyruvate reaches a certain level. Due to this, pyruvate from glucose is not produced in excessive quantities. Fructose is also converted to pyruvate, but thanks to another enzyme – ketohexokinase (fructokinase). However, the activity of this enzyme is not limited by the high concentration of the end products of the reaction, and continuously increases in parallel with the concentration of fructose *.
Due to this, an excess of fructose in food generates an excess of pyruvate. Excess pyruvate is then converted to fatty acids, and fat is deposited in various parts of the body. With the growth of body fat, the level of inflammation increases – both local and general. Fat also causes an increase in estrogen levels and inflammation of the walls of blood vessels. Metabolization of fructose is accompanied by the production of large amounts of uric acid, as well as methylglyoxal, which inhibits mitochondrial respiration of the cell.
However, the differences in simple carbohydrate metabolism begin to become important as total calories increase *. In a case-control study of 180 women with breast cancer, the association of relative cancer risk adjusted for age, body mass index, smoking, alcohol consumption, physical activity, and dietary intake of calories, proteins, and fats was analyzed. Positively associated with breast cancer were: the amount of simple carbohydrates consumed (OR=1.76), sucrose (OR=1.97), maltose (OR=4.07) and fructose (OR=1.104). However, no significant association was found between breast cancer and consumption of glucose, galactose, and lactose *. These data allow us to reasonably adjust our diet.
For example, a food sugar molecule (sucrose) is made up of a unit of glucose and a unit of fructose, while a starch molecule is made up of many units of glucose alone. Fructose is worse than glucose; from this position food sugar is worse than starch. Sucrose is metabolized to glucose and fructose, and fructose causes elevated serum triglycerides, insulin resistance, and hyperglycemia *, and each of these factors contribute to cancer. A simple example: as a result of metabolism, fructose can be converted into fatty acid – palmitic acid, which can independently activate one of the pathogen-recognition receptors (TLR4), thereby triggering a cascade of immune reactions *.
Several observational studies have confirmed a positive association between elevated fasting blood sugar and breast cancer risk. In premenopausal women at 95 mg/dL, this risk was half that of women at 74 mg/dL *. In another case, blood sugar levels > 84 mg/dL were twice as likely to cause breast cancer compared to levels < 71 mg/dL *. In another study, women with blood sugar levels < 100 mg/dL had a one-quarter lower risk of developing breast cancer compared to women with levels between 100-125 mg/dL *.
Elevated fasting blood glucose is a risk factor not only for breast cancer * but also for several other major cancers * and most other degenerative diseases. For example, the relative risk of Parkinson's disease increases 3-fold with a high sugar intake and 5-fold with a high fat intake *. Since sucrose is a significant source of glucose in the modern diet, elevated blood glucose levels may indirectly indicate excessive fructose intake.
Fructose causes a noticeably lower release of insulin into the blood compared to glucose, and for this reason it is sometimes recommended for diabetics. However, fructose ingestion causes changes in the endocrine system that can potentially promote increased energy intake and weight gain by decreasing levels of insulin and leptin, two hormones that suppress food intake *. In addition, fructose worsens the post-meal decline in ghrelin levels, the hunger hormone, which stimulates an increase in food intake * *. Thus, fructose promotes excessive calorie consumption.
Sucrose intake and total carbohydrate intake at 10-19 years of age are also associated with higher mammographic breast density at 25-29 years of age. The difference is approximately 24% between the groups with the lowest and highest consumption of sucrose *. This should not be surprising since mammographic density is associated with levels of low-grade systemic inflammation. And it is largely fueled by fructose, because per unit mass, fructose, in comparison with glucose, produces 100 times more reactive oxygen species *.
Replacing fructose with an energy-equivalent amount of glucose improves insulin resistance and uric acid levels *. Even with the same caloric intake, reducing the share of sugar in total calories to 10% and fructose from 12% to 4% dramatically reduced liver fat production, decreased visceral fat stores, and improved insulin kinetics in obese adolescents in just 9 days *.
Interestingly, all artificial sweeteners that were intended to be healthier alternatives actually produce the same signaling effects in the body and lead to an even higher risk of metabolic syndrome than natural sugars *. Replacing sugar with honey also does not solve the sucrose problem. If sugar contains equal amounts of sucrose and glucose, then honey contains more sucrose than glucose (the more sucrose in honey, the faster it sugars). Because of this, honey is no healthier than sugar. On the other hand, honey contains a certain amount of phytonutrients that have a positive effect on human health. And if there is a choice between sugar and honey, then for this reason, it is apparently better to choose honey.
The complex carbohydrates (polysaccharides) found in foods such as whole grains, pseudograins, and legumes provide a lower glycemic load for the same energy value than simple carbohydrates. They saturate the body with glucose more slowly than simple carbohydrates, because they require preliminary enzymatic breakdown, and it takes a certain time. The extended metabolism of complex carbohydrates allows you to feel full for a longer period, and provides a longer supply of energy.
Therefore, it is not surprising that simple and complex carbohydrates have different effects. A high proportion of simple carbohydrates in the diet increases inflammation, while a high proportion of complex carbohydrates, on the contrary, reduces them *. In postmenopausal women, simple carbohydrates lower sex hormone-binding globulin (SHBG) levels, while fiber increases them *. Replacing fructose and sucrose with starch reduces fasting glucose, low-density cholesterol (LDL), glycated hemoglobin (HbA1c), insulin resistance (HOMA-IR), uric acid, C-reactive protein (CRP), alanine transaminase (ALT), aspartate transaminase in humans (AST) and liver fat content *.
There are also differences between complex carbohydrates in their effect on the body. As with proteins, fats, and simple carbohydrates, the source of complex carbohydrates and their quality matter. Excessive intake (more than 220 g/day) of easily fermentable carbohydrates (hulled rice and wheat) and from starchy foods (potatoes) is more associated with metabolic syndrome and hyperlipidemia than intake of carbohydrates from other sources (legumes, vegetables, dairy products, etc.) *. Starchy carbohydrates are associated with increased levels of visceral fat and serum triglycerides, while in some studies they have been negatively associated with HDL cholesterol *. At the same time, whole grains reduce the risk of metabolic syndrome and diabetes *.
Of course, even complex fermentable carbohydrates sooner or later also turn into glucose, the excess of which, as already mentioned, increases the risk of cancer * and cardiovascular diseases *, atrophy of important parts of the brain * *, as well as degeneration of the body as a whole. However, the conversion of complex carbohydrates to glucose is a lengthy process, and therefore does not create high peak rates and, accordingly, the risks of these diseases.
In addition, we can significantly reduce our insulin response to grains simply by changing our food choices. We can take whole grain cereals instead of refined flour; to eat durum wheat pasta instead of a lush baguette; to cook porridge not from ground large grains (wheat, rye, oats), but from whole small ones (flax, false flax, chia, quinoa).
Fiber, found in both vegetables and whole grains and beans, slows down the absorption of nutrients from the intestines, allowing you to flatten the blood glucose saturation curve. In fact, increasing your fiber intake, rather than just reducing your carbohydrate intake, is the key to lowering postprandial blood glucose release.
Insoluble non-starch polysaccharides (such as cellulose) increase food mass due to their bulk, as well as their ability to absorb and retain water, which provides a feeling of fullness with fewer calories. In addition, fiber binds many toxins and bile acids, and speeds up the process of passage of consumed food through the intestines.
Fiber, together with a low-fat diet, reduces estradiol levels without adversely affecting ovulation *. It has been observed that vegetarians, with their high fiber intake, are better at getting rid of carcinogenic estrogen metabolites. Instead of being absorbed back into the blood, they are excreted in the feces, thereby reducing the concentration of estrogen in the blood plasma * *.
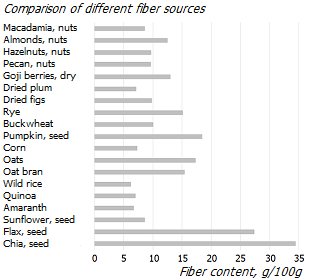
Fiber may reduce the risk of breast cancer * *, especially for ER–/PR–-tumors *; while low fiber intake may lead to an increase in tumor size *. Interestingly, while the consumption of fruits and vegetables is associated with a reduced risk of breast cancer, the consumption of juices from these fruits, on the contrary, is associated with an increased risk *. This supports the idea that fiber is the key factor in this difference. However, the types and sources of dietary fiber have different effects on risk reduction *, possibly due to their uneven effect on the bacterial profile of the gut microflora.
Non-fermentable complex carbohydrates are not nutrients because they are not absorbed by the body. However, they are food for bacteria that colonize the intestines. By fermenting fiber, intestinal bacteria such as Clostridium butyricum, Roseburia intestinalis and Faecalibacterium prausnitzii secrete, among other things, short-chain fatty acids – acetic, propionic, butyric and valeric acids.
Short-chain fatty acids produced by gut microbes not only provide us with additional calories. Propionic acid (propionate) increases insulin sensitivity * and reduces appetite *. And butyric acid (butyrate) is known for its ability to significantly reduce the risk of all types of cancer by suppressing the growth of cancer cells, as well as by stimulating their apoptosis and differentiation.
In premenopausal women, a high intake of soluble fiber (and naturally associated phytonutrients) is associated with an incredibly high relative risk reduction for the most dangerous breast cancer, the ER–-subtype *. Every additional 10 g/day of plant fiber is associated with a 14% reduction in premenopausal breast cancer *. Dietary fiber intake of 40 g dry weight per day reduces the risk of breast cancer by about 25% compared with its intake of 25 g (a level that is typical for «wealthy», disadvantaged countries) *. It can be expected that an increase in fiber intake to levels characteristic of primitive man (100 g/day) will reduce the risk of disease even more significantly.
The source of plant fiber also matters. Grain fibers, especially soluble fibers, show slightly more benefit than vegetable and fruit fibers *.
As already noted, reducing dietary fat intake at the same time as increasing fiber intake actually means a change in the structure of fatty acids absorbed by the body: import long-chain molecules are replaced by domestic short-chain ones. Thus, we bring the diet of modern man closer to the diet of human ancestors.
Again, carbohydrates found in whole (unrefined) foods have a richer nutritional profile than carbohydrates found in refined foods (pasta, white flour, etc.) that are free of fiber, vitamins, minerals, beta-glucan, and food antioxidants.
Therefore, the consequences of consuming certain sources of complex carbohydrates can be different. For example, a diet high in refined carbohydrate sources (pasta and rice) can speed up the onset of menopause by a year and a half earlier than the average age. And diet high in unrefined sources of carbohydrates (legumes) as well as fatty fish may, on the contrary, delay the onset of menopause *.
We can evaluate the pros and cons of accelerating the onset of menopause in different ways. Women with early menopause have an increased risk of osteoporosis and heart disease, and women with late menopause have an increased risk of breast, uterine, and ovarian cancer associated with high estrogen levels. However, a high intake of refined carbohydrates in itself raises the risk of breast cancer. In any case, the consumption of unrefined sources of carbohydrates will be more beneficial.
The high carbohydrate diet that will be suggested below does not mean a high glycemic diet, but a diet high in plant fibers. The main source of energy should be vegetables, whole grains and legumes. They are rich in fiber and contain complex carbohydrate molecules that provide a low glycemic index and are also a major source of micronutrients and phytonutrients. At the same time, the consumption of simple carbohydrates and other foods with a high glycemic index should be minimized.
Criticism of a high-carbohydrate diet. Recently, a massive information attack on a high-carbohydrate diet has been intensifying, in which, unfortunately, some of the medical workers are also participating. In this campaign, it seems that the baby is thrown out of the bath along with the water. The main complaint against carbohydrates is that they cause a temporary increase in blood insulin levels, with all the ensuing detrimental consequences discussed above.
At first glance, the negative assessment of a high-carbohydrate diet looks fair. However, a deeper penetration into the topic reveals the fact that the opponents have primitivized the problem, and even the substitution of concepts in the course of the dispute.
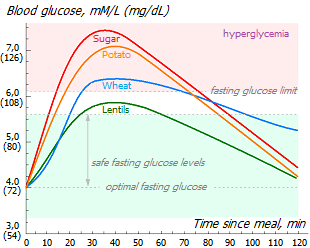
Indeed, in the graph shown here, it is observed that the consumption of a high-carbohydrate meal naturally raises blood glucose (and, by extension, insulin). However, the magnitude and duration of the rise depends on the quantity and quality of the content, as well as on consumption with other other foods.
Given the same amount of consumption, the highest spikes in sugar (and insulin) come from simple carbohydrates found in sugary and refined grain products. A fluffy white flour bun with a cup of sweet tea after dinner with potatoes is sure to bring on acute hyperglycemia and an insulin storm. Starchy vegetables alone generate a slightly lower wave. Legumes (in reasonable amounts) help avoid hyperglycemia, and vegetables allow you not to go beyond the safety limit at all, regardless of their amount consumed. The less refined carbohydrate products, the more fiber they contain, the weaker the insulin surge they create.
The addition of vegetables, dark green plants to complex carbohydrates, as well as the fiber contained in the grain shell, or the lignans contained in the seed of flax or fenugreek, inhibits the absorption of carbohydrates. This dampens the insulin surge, stretching it over time; especially if the food does not contain many calories. Thus, a healthy diet, i.e. a low-calorie diet based on vegetables, legumes, whole grains, with a small amount of «good» fats and «good» proteins, does not generate excessive insulin levels.
At the same time, high-calorie and/or high-glycemic foods, frequent high-calorie snacks between meals, late dinners, and some other unhealthy eating habits can cause chronic hyperglycemia, and with it high insulin levels and insulin resistance of cells. However, opponents are quick to put the blame for this on carbohydrates in general, without delving into the essence of the problem.
One would certainly agree with critics of the high-carbohydrate diet if they used the expression «high-glycemic» or «high-fructose» diet instead of «high-carbohydrate» diet. If only opponents criticized the high content of easily digestible simple carbohydrates in food, and would not lump sugar, starch and fiber into one pile. It seems that such a replacement would remove many controversial issues and confusion in this matter. Ultimately, it is hyperglycemia that causes breast cancer risk, not the amount of available carbohydrate in a diet *.
For example, although the food of higher primates consists almost entirely of carbohydrates, they do not suffer from the so-called «diseases of civilization», including diabetes. Because most of the wild plant foods that make up their diet are high in fiber, but low in sugar and calories. In other words, this is a high-carbohydrate, but low-glycemic diet. At the same time, the tragic example of the Inuit shows that a high-glycemic diet significantly increases the risk of both diabetes and cancer.
In the diet of Late Paleolithic people, complex carbohydrates (mainly from vegetables and fruits) provided between a third and a half of all calories, although the exact figure varied by region and season *. In the modern diet of residents of «wealthy» countries, there are much more carbohydrates, with the majority being simple carbohydrates, mainly sucrose. Compared to the «Paleolithic» diet, the «Western» diet has 3 times less vegetables and fruits, and only vegans come close to an adequate level of their consumption.
Carbohydrate opponents promote unnatural diets high in fat or protein with the good intention of reducing post-meal blood glucose spikes by taking longer to metabolize fats or proteins than carbohydrates. However, clinical comparisons of low-carbohydrate and low-fat diets available to date do not give grounds to assert that in the long term a low-carbohydrate diet provides more pronounced benefits for the body * * * * * * *.
In an attempt to prove the fundamental harm of carbohydrates, manipulations are sometimes used. In addition to not making a distinction between high and low glycemic foods, they is not made between whole and refined carbohydrate sources; between a meal with only carbohydrates and a meal that combines carbohydrates with vegetables; between low-calorie and high-calorie diets; between the nutrition of healthy and sick people; etc. For this reason, the results of many observational studies lead to biased conclusions.
Of course, any carbohydrates change the concentration of glucose in the blood, and with it, insulin. However, daily fluctuations in insulin levels are as natural as daily fluctuations in cortisol and melatonin levels. Glucose and insulin create the risk of developing degenerative diseases only when a certain threshold is chronically exceeded. That is, you need to aim for a safe level of glucose in the blood, and not for a low consumption of carbohydrates. And these are, although related, but not equivalent goals. If our task is to keep glucose levels within safe limits, then we need to intelligently organize our nutrition and physical activity in order to avoid spikes in it, and not to get rid of carbohydrates fundamentally. To do this, you should reconsider the ratio of simple and complex carbohydrates in food in favor of the latter.
Conclusions. A review of the 92 most common foods and their association with breast cancer risk showed that the greatest benefits for postmenopausal women come from vegetables, fruits and carbohydrates, and especially dietary fiber. And the greatest danger comes from alcoholic drinks, of which dry red wine is the least evil (beer and cider are worse) *. Women who eat very few vegetables versus women who eat a lot of vegetables have a significantly higher risk of breast cancer *. The relative risk of ER-subtypes of cancer increases in such women by 30%, and ER– subtypes by 40%.
The Academy of Nutrition and Dietetics considers an adequate intake of 14 g of total fiber per 1'000 kcal of food intake, i.e. ~ 25 g for adult women and ~ 38 g for adult men *, which is one and a half times higher than current consumption in European countries. But in fact, even these values can be underestimated. In modern hunter-gatherers, as in primitive people, fiber intake is many times higher (> 100 g/day) *.
An analysis of the change in nutrition of 11 non-European populations from their traditional diets to a «Western» diet showed that the increase in non-communicable chronic diseases among them was associated with an increase in the consumption of refined carbohydrates to a greater extent than with an increase in calorie intake, a decrease in physical activity, or other risk factors *. This included Yemenite Jews, Tokelauans, Tanushimaru Japanese, Maasai, Pima, Navajo, Aboriginal Australians, Inuit, Hadza, South African Natal Indians and Zulu speakers.
The American Cancer Society and the American Society for Clinical Oncology recommend a plant-based diet, whole grains, legumes and ocean fish * *. This recommendation is supported by systematic reviews of different types of diet * *. However, in individual cases, such as severe diabetes, these recommendations may be revised.
In a metaanalysis of 8 prospective international studies with a follow-up period of 7 to 26 years, and involving more than 400'000 overweight people, the lowest all-cause mortality was associated with an average carbohydrate intake in the diet of ~ 50-55% of the total daily intake energy (%E). A low-carbohydrate diet (20%E from carbohydrates) increased the risk of mortality linearly by 50%, while a high-carbohydrate diet (80%E from carbohydrates) increased the risk of mortality by 10% *. At the same time, it was noted that the replacement of carbohydrates with animal proteins or fats increases mortality, while the replacement of carbohydrates with vegetable proteins, on the contrary, reduces it.
A special systematic review showed that patients diagnosed with cancer would certainly benefit from a low-fat, nutritious diet, regular intake of fiber and vegetable protein, while a Western diet and a high intake of saturated fats may, on the contrary, increase the risk of mortality *. Low-carbohydrate diets are associated with a significantly higher risk of all-cause mortality * and worse overall health * *. At the same time, low-fat diets are correlated with a reduced risk of breast cancer and an improved prognosis for women with already diagnosed breast cancer * * * *.
In animal studies, both the calorie-restricted diet and the low-protein, high-carbohydrate, without calorie restriction diet equally increased lifespan and improved metabolic parameters such as insulin, glucose, and blood lipids. High-carbohydrate, low-glycemic diets have demonstrated the metabolic benefits of calorie restriction even without an actual 40% reduction in calories *.
However, the conclusions drawn from these studies may be somewhat oversimplified. In fact, overall mortality and dietary carbohydrate intake have a complex relationship that is highly dependent on calorie content, macronutrient quality, and dietary sources *. Perhaps this is the reason why the different design of observational dietary studies can lead to ambiguous conclusions.
The German Society of Nutrition suggests that 50% of all energy should come from carbohydrates, of which a fifth should be simple sugars *. And the US Institute of Medicine allows for a wider range – of 45-65% of all energy from carbohydrates *.
Summarizing the above, we can come to the following conclusions:
It would be prudent to reduce total calorie intake to the physiological minimum and also avoid diets that create a hyperglycemic state.
High calorie intake may be a more significant risk factor than the macronutrient ratio of the diet.
As the total calorie content of food increases, the macronutrient ratio becomes more and more influential.
Regardless of the structure and calorie content of macronutrients, nutrition should provide the body with sufficient amounts of micronutrients.
The balance of food is determined by the ratio of the main food components.
The human body has a high metabolic flexibility, and is able to use a wide variety of food sources. He is able to survive long periods of winter hunger due to the fat reserves accumulated in the summer. It is able to tolerate both high-fat, high-protein, and high-carbohydrate diets; and easy to switch from one to another. However, tolerance does not mean optimality.
The bar chart below shows the association between the balance of macronutrients in the total caloric intake of different countries of the world. Here, countries are ranked vertically in order of incidence rate, and absolute values of the calorie intake and the share of each of the macronutrients in it are compared horizontally. It is obvious that the calorie content of nutrition is growing from the ten most prosperous countries in terms of morbidity (the «green10») to the ten least prosperous (the «red10»).
However, it can be seen that in the «red10» group, with a 15% increase in calories, weight intake of carbohydrates fell by 14%, weight intake of protein rose by 10%, but weight intake of fat skyrocketed by 86% †. Thus, as the statistics worsen, the total calorie content grows mainly due to fat. This change in diet leads to strong imbalances between macronutrients.
Therefore, in the ten most prosperous countries, the average median ratio of fats to carbohydrates is 1:3, while in the ten most disadvantaged it is twice as bad – 1:1.4. This almost quadruples the risk of cancer.
Once more, both the increase in caloric intake and the increase in calorie-related incidence of breast cancer is mainly due to an increase in fat intake.
The following graphs show associations between macronutrient energy ratios and breast cancer risk.
From these graphical comparisons, it can be assumed that the less fat in the food, the lower the risk of cancer. The lowest morbidity rates are observed at a calorie ratio of carbohydrates:fats of 1:3. The level of protein intake is also associated with cancer risk; the lowest incidence rates are observed at a caloric ratio of carbohydrates:proteins of 1:6.5 and fats:proteins within 1:1.5. These numbers provide us with a foundation to balance the macronutrients of a diet that can be said to be safe in terms of breast cancer risk.
So, the balance of macronutrients is as important for health, if not more, than the absolute indicators of their consumption *. It is known that violations of the following ratios are expressly associated with an increase in the risk of breast cancer:
- carbohydrates : fats in favor of fats;
- carbohydrates : proteins in favor of animal proteins;
- vegetable : animal fats in favor of animals;
- saturated : unsaturated fats in favor of saturated;
- PUFA ω-6 : PUFA ω-3 in favor of ω-6;
- medium chain : long chain fats in favor of long chain ones;
- simple : complex carbohydrates in favor of simple ones;
- fiber : the amount of food in favor of the latter.
A growing body of evidence indicates that even common foods consumed daily, and not considered carcinogenic, can contribute to the appearance and development of breast cancer if the amount and balance of their consumption is disturbed. This applies not only to fats and milk. The graph shows that with an increase in the proportion of protein in the diet, the risk of morbidity increases. Each additional serving of chicken eggs per week can increase the incidence by 31%, and each additional serving of red meat (100 g) per day by 56% * *.
However, in our reality, the absolute consumption of animal protein is growing at the same time as the absolute consumption of animal fat, because farm meat contains it in large quantities. The question arises which is actually more dangerous – protein or fat.
The last graph †: provides the answer: the higher the fat:protein ratio, the higher the risk of breast cancer. As we can see, the relationship does not look linear. The fatter the meat, the more dangerous it is. A sharp change is observed in the region of the ratio of fats:proteins 2.5:1. The lowest risk is observed at the following ratios of calories:carbohydrates:fats – 3.5:1; carbohydrates:proteins – 6.5:1; fats:proteins – lower than 2.3:1. In terms of dry weight, these ratios will be: carbohydrates:fats – 8:1; carbohydrates:proteins – 6.5:1; fats:proteins – lower than 1:1.
The last table shows that, regardless of total caloric intake, the critical dietary risk factor for breast cancer is the carbohydrate:fat ratio. The higher it is, the lower the risk of breast cancer. Spain and Greece may seem like exceptions, if you forget that in these countries the largest proportion of fats is olive oil, not saturated fats. A rather mysterious exception is Uruguay, where there are no negative dietary factors for such a high incidence.
Of course, both the methodology of the results obtained and the conclusions drawn from them can be called into question, since several interrelated variables and their combinations in the food taken by a person are involved here *. The more complex the combinations involved, the more difficult it is to make sure that the association shown is stronger than chance.
Therefore, it would be more correct to speak not only and not so much about the absolute levels of consumption of individual foods, their ratios and combinations, but about ready-made nutrition models, such as «Paleolithic», «Japanese», «Mediterranean» or «vegan». It remains to be seen which of them maximally reduces the risk of morbidity and mortality from cancer.
Every month, new publications appear, refuting all previous opinions and dietary recommendations, and confusing the reader's head. Every year, nutrition gurus tout more and more diets that are supposed to be the «ultimate» diet. This game continues indefinitely, and does not bring us any closer to the fundamental conclusions. Instead, it only causes confusion, disorientation, loss of credibility in publications, and following of false prophets.
There is a subjective opinion of magazine experts and popular authorities. And there are dispassionate statistics. There are one and a half hundred countries in the world that provide a report on domestic food consumption. And each of these countries has unique dietary characteristics, which are displayed in a special table †. To simplify the picture, only forty countries were selected. The choice fell on the most significant, or those with the largest deviation from the average curve on the graph of the dependence of the risk of disease on caloric content.
A review * of the nutrition structure of the population of various countries * of the world shows that the top ten countries with the lowest incidence of breast cancer have the following characteristics:
• the ratio of calorie carbohydrates to fats in the diet ranges from 11.7:1 to 3.5:1;
• the ratio of calorie carbohydrates to proteins in the diet ranges from 5:1 to 7.5:1;
• the weight ratio of raw vegetables to dry cereals ranges from 1:1 to 4:1;
• the ratio of unsaturated fats to saturated fats – not less than 8:1;
• share of polyunsaturated fats (PUFA) in total calories – about 7%;
• ratio animal proteins to vegetable proteins – 1:2.5;
• total consumption of sugar, including in a latent form – no more than 30 g/day;
• consumption of fish and meat – up to 80 g/day, eggs – 25 g/day, fiber – at least 25 g/day, dairy products – in the equivalent of 200 mL/day of whole milk.
Such data can be used as nutritional recommendations with an average calorie intake of 2'880 kcal/day observed in these countries. The lower the calorie content of nutrition, the less significant the question of the balance of macronutrients in human food becomes. When calories are reduced below the physiological minimum (< 1'600 kcal/day), macronutrient ratios will be a minor issue. The main metabolic problem in conditions of scarcity of resources is their most efficient use.
A manipulation study comparing the effects of two low-calorie (1'500 kcal/day) diets, low-fat and low-carbohydrate, found no significant differences in most markers of inflammation * and markers of cardiovascular disease *. In another case, a high-fat (energy ratio of carbohydrates:proteins:fats – 14:28:58) and high-carbohydrate (respectively, 53:17:30) diets were compared. With a reduction in total calorie intake to 500-1'000 kcal/day, both of variants almost equally improved clinical glycemic control and cardiovascular risk markers in patients with type II diabetes *.
In obese women, reducing caloric intake to 1'200-1'340 kcal improved health outcomes equally in both high-protein and high-carbohydrate diets * *. The same was found when comparing high-protein and high-fat diets with a reduction in calorie intake to 1'430 kcal *. Both the first and second cases dealt with anti-obesity therapies, which cannot be considered as regular diets. Therefore, when we do not limit ourselves in the amount of food we eat, it is still worth adhering to the balance of macronutrients recommended above and the caloric content range of 1'600-2'500 kcal/day.
The fact that the structure of the diet proposed here is based not on manipulative, but on observational studies of the national diets of various peoples of the planet, which are subject to the influence of extraneous factors, should not confuse us. The greater the number of cases involved in the statistics, the stronger the concomitant factors cancel each other out, and the less influence they have on the reliability of the result.
It is important to note that the diet suggested here is preventive. In the case of already existing cancer, we may have to resort to therapeutic rather than preventive diets for the duration of treatment.
The method of cooking significantly affects the quality of food, and with it, human health. A high ratio of fried to cooked foods has been linked to an increased risk of both malignant and benign breast tumors. With the same amount of the original food product, women who consume fried foods more than 2.5 times more often than boiled ones, compared with women who consume them equally, increase the risk of malignant tumors by 1.5 times, and benign tumors by 3.6 times times. And even the correction for other distorting factors has little effect on this ratio *.
Although heat treatment improves the absorption of food, at the same time it depletes food of many useful components. High-temperature processing with fats (roasting) or roasting on fire is accompanied by decomposition of fat and the formation of some carcinogenic compounds, such as polycyclic aromatic hydrocarbons and aldehydes. They create a pleasant aroma, stimulate appetite and add flavor to cooked food, but their systematic consumption increases the risk of cancer *.
Thus, an increase in the consumption of well-done red meat is associated with an increased risk of breast cancer *, especially in women with a higher body mass index *. This risk also increases in postmenopausal women *. Eating fried meat may increase the relative risk of breast cancer by 1.7 times for all women, and by 3 times for postmenopausal women *.
The mineral balance of food is just as important to the body as the balance of essential nutrients and micronutrients. First of all, it concerns the balance between intracellular (potassium and magnesium) and extracellular (calcium and sodium) electrolytes. The K:Na ratio in food should be > 1,5; Ca:Mg ~ 2,4; Ca:P ~ 2; Ca:K ~ 0,3; Na:Mg ~ 5,5; I:Se ~ 2,5-3; Cu:Fe ~ 110.
Although this is not easy to do in practice, satisfactory ratios can be achieved by more thoughtful food selection. For example, chia seed is a rich source of readily available calcium, making it an attractive dairy alternative.
At the same time, ensuring the balance of micronutrients is more difficult than ensuring their absolute value. Some software products can facilitate the solution of both the first and second tasks. After analyzing your weekly diet, you can easily estimate the approximate intake of certain substances. An example is the Russian-language online calculator «My Healthy Diet» *.
If it is not possible to ensure the mineral balance through diet, we still have the opportunity to achieve it by taking appropriate supplements. Their dosage can also be approximately calculated using the same software product.
However, one should not forget about the absolute values of consumption. For example, high salt intake accelerates the growth of breast cancer and promotes lung metastasis *. It is also not worth making a tragedy of the fact that an acceptable balance cannot be achieved, although absolute consumption turned out to be sufficient. For most of the substances required by the body, a simple principle applies: a deficient product is absorbed much better than an excess.
Acid load. After being ingested, digested and metabolized, foods can produce acidic or alkaline waste products that enter the systemic circulation and create an acidic or alkaline load, respectively *. The metabolism of fats does not produce an acidic or alkaline load, but this is not the case with carbohydrates and proteins.
The by-products of carbohydrate metabolism are water and carbon dioxide, which, when combined, form carbonic acid having a weak acidity (pH 3.7 at 100 mM). Carbonic acid is unstable, and easily breaks down again into water and carbon dioxide, which is then excreted mainly through the lungs.
By-products of protein metabolism are highly acidic acids – nitric (pH 1.1), phosphoric (pH 1.6) and sulfuric (pH 1.2), which are then excreted through the kidneys. When too many acidic products are produced in the body and the kidneys cannot remove them efficiently, a condition called metabolic acidosis occurs.
Early humans consumed sufficiently large quantities of alkaline-loading plant foods to balance the acid load created by meat foods. In great apes, closest to man and having a common ancestor with him, from 88% to 97% of all food is plant food *, which is infinitely far from the consumption of raw plant foods by modern man. Of course, the evolutionary move away from the all-vegetarian food of human ancestors led to some anatomical changes in the human body. However, the metabolic changes that have taken place during this time are not so large-scale as to be able to reduce the share of vegetables in food to the negligible level that we observe today in European countries.
Modeling of the diet of the East African ancestors of Homo sapiens shows that it produced a predominantly alkaline load *. Calculations of food acid load in 229 historically studied hunter-gatherer societies around the world showed that about half of them were dominated by acid load, and half were alkaline *. Finally, the modern human diet in «rich» countries creates a high acid load *.
Violation of evolutionarily established and genetically determined nutritional needs causes chronic low-level metabolic acidosis – an excess of acid-forming chemical elements and acid metabolites in the body *. This leads to an overload of the main mechanisms for compensating for acidosis – respiration, sweat, feces and urine, resulting in bad breath, skin defects and kidney stones of various nature. However, the matter is not limited to this.
The body strives to keep the acidity of the blood at a pH of 7.4±0.05 so that the blood can hold enough oxygen and the enzymes can function adequately. To ensure this value, the so-called «allkaline buffers» in the blood bind to excess acids and quickly neutralize them. A chronic excess of acids leads to the depletion of alkaline buffers, and then the second regulation strategy comes into play: excess acid products are dumped from the blood into organs and tissues.
Alternatively, alkaline elements are drawn in the opposite direction, from the tissues into the blood, to compensate for the chronic acidosis. For example, bone tissues are deprived of calcium, which can cause dental disease. Other tissues can also lose alkaline elements, receiving acid-forming molecules in return, and gradually become acidic. A high dietary acid load is more likely to lead to diabetes, hypertension, brain damage, and an increased risk of cardiovascular disease *.
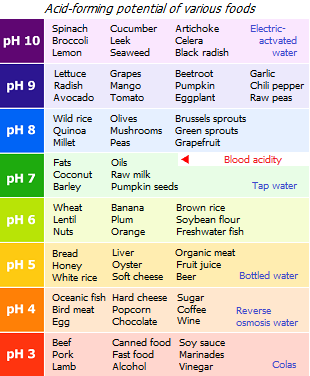
The widespread diet of modern man, commonly referred to as the «Western diet», creates a chronically elevated acid load. This can contribute to common age-related changes such as weakening of the skeleton (osteoporosis), tooth decay and loss of muscle mass (sarcopenia). Tissue acidification promotes cell mitosis and increases the risk of cancer, and also negatively affects the activity of many biochemical factors and enzymes *. When the reserves of alkaline elements in the tissues are significantly depleted, it becomes more and more difficult to maintain adequate blood acidity. It begins to rise, and the oxygen content in the blood begins to fall, which increases the risk of degenerative diseases.
An increased acid load caused by an unhealthy diet may also be a significant risk factor for breast cancer. This is especially true for ER-negative types of tumors, and to an even greater extent – triple negative type of cancer (TNBC). Conversely, an alkaline diet can reduce the acid load on tissues, playing a protective role *.
Vegetables, fruits, their juices, herbs, bananas, potatoes, as well as alkali-rich and phosphorus-poor drinks have a negative acid, i.e. alkaline load. Grains and legumes create a low acid load, which can be easily offset by eating vegetables. Meat and dairy products, fish, and drinks high in phosphorus (such as Coca-Cola, cocoa) create relatively high acid loads *.
The pH values of various products shown in the figure above do not mean that these products have the acidity indicated in it. They note how strong the effect these products have on the acidification or alkalization of tissues. For example, lemon is very sour in taste, and has a high acidity index; however, its metabolites create an alkaline load.
PRAL (Potential Renal Acid Load) is currently the most commonly used indicator to assess the acid-forming capacity of foods. You can compare the PRALs of different products using the included table †. Although many healthy foods (nuts, fish, chocolate) have an acidifying effect, this does not mean that they should be completely avoided. This only means that their intake should be balanced with an appropriate amount of products with an alkalizing effect.
The «Healthy Diet» Weekly Set below †, with its abundance of vegetables, is capable of producing at least -150 mEq per 100 g of product daily, which will provide a weak alkalizing effect of this diet.
The inflammatory load, caused by food is one of the key causes of almost all degenerative diseases, not just cancer. Healthy foods are anti-inflammatory foods. Known dietary factors that promote inflammation are an increased ω-6:ω-3 fatty acid ratio *, a high intake of total fats, meat, and simple sugars *, and individual intolerance to certain dietary proteins such as gluten *, germ agglutinin wheat * and other lectins.
With less than 1% of the population having severe gluten and no more than 3% non-gluten sensitivity to grains *, for the rest of the population avoiding grains is not justified *, and may be harmful. In particular, the exclusion of grain fiber and polysaccharides from the diet due to the transition to a gluten-free diet reduces the diversity of the intestinal microflora *. In any case, it would be advisable to test yourself for latent gluten and casein sensitivities before committing to such restrictions in your diet.
Humans have consumed gluten for thousands of years, but only in recent decades has gluten sensitivity become increasingly widespread. A significant part of this problem is caused not so much by gluten or casein itself, but by other elements that bind to these proteins, for example, pesticides, herbicides and other chemical agents used in agriculture and the food industry. The resulting changes in the structure of the protein, which make it look like the natural targets of antigens present in the body, enhance immune and inflammatory responses. In view of this, the desire to consume the so-called «organic» food is welcome.
Insulin and glycemic load are the result of a high consumption of simple carbohydrates such as dietary sugar and, in response to this, a sharp release of insulin into the bloodstream. High levels of circulating insulin and insulin-like growth factor (IGF-1) are known to be growth factors for most cancer cells * * *.
A meta-analysis of prospective studies showed a significant positive association between glycemic index, carbohydrate quality score, and breast cancer risk *. Especially high positive associations have been observed between a high dietary glycemic load and the risk of ER– and ER–/PR– breast cancer in postmenopausal women *.
Therefore, it is recommended that, as much as possible, reduce the consumption of simple carbohydrates, such as sugars, in favor of complex carbohydrates that undergo a long period of metabolism, such as legumes and whole grains. This will avoid sudden releases of insulin into the blood and provide a more stable level of glucose. Fiber, contained in vegetables and grain shells, also somewhat delays the entry of simple sugars into the blood.
The frequency of meals can significantly affect the stability of blood glucose levels and keeping them in a relatively safe range.
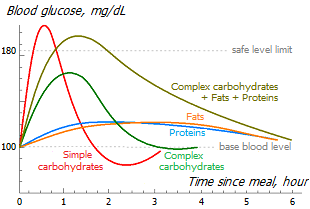
As you can see from the graph here, simple carbohydrates (sugars) quickly create high blood glucose levels, and in response to this, a massive insulin surge can lower glucose levels below the original level, causing hunger. If you take fast-digesting carbohydrates again to satisfy it, a kind of «swing» is created, throwing blood glucose levels from extremely high to extremely low.
Complex carbohydrates require pre-enzymatic processing, and therefore their glycemic load is stretched over time, reducing the height of peak blood glucose saturation, and providing the body with energy for a longer time. Carbohydrates in a denser, compact form (unleavened bread, pasta) also require a longer period of their assimilation compared to carbohydrates in a porous form (leavened bread) *. An even smaller release of glucose comes from whole grains or coarse grains, which have much less outer surface and cover carbohydrates much deeper than finely ground grains and flour. Due to this, the release of insulin becomes less intense, and the balance between glucose and insulin is more adequate.
Proteins and fats take even longer to metabolize than complex carbohydrates and can make us feel full longer. At the same time, the production of cellular energy from fats and proteins is less efficient than from carbohydrates, because their metabolism requires more energy.
The combination of carbohydrates+proteins+fats+fiber allows you to maximize the time between meals. In this case, the level of glucose in the blood can be kept in a relatively safe range.
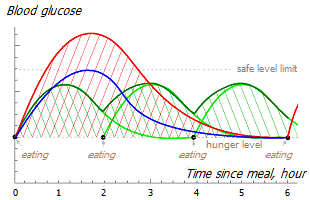
It is easy to imagine that frequent meals of low-calorie foods will create a lower and more uniform glycemic level than infrequent meals of high-calorie foods.
The same amount of energy input (shaded area under the curve) in one case temporarily but strongly takes the glucose level beyond the safe level (red curve), and in the other case keeps it within reasonable limits (green curve).
However frequent small meals make sense when a high enough amount of calories are consumed with food, and we are forced to break up spikes in glucose levels into smaller parts. If the total calorie intake is reduced to the physiological requirement, then its benefits disappear. In this case, it is possible to keep the blood glucose level at a satisfactory level by following the usual 3 meals a day, but low-calorie meals (blue curve).
In addition, the more often we eat, the more likely we are to exceed the daily calorie limit. The longer the gap between meals, the more metabolic flexibility cells develop (the more easily they switch from one energy source to another, for example, from glucose to ketones). There are other reasons to refuse frequent fractional meals or snacks between meals, even if they are low in calories. The more often food enters the stomach, the worse the subsequent metabolic response to it.
However, if we are not talking about fasting, meals should be regular. Irregular («ragged») food intake can increase the relative risk of breast cancer in women by 2.2 times compared with regular intake *.
Food personalization. Even the most compelling nutritional advices can be challenged by personal examples. A natural question arises: why does the same diet cause different reactions in different people? For example, under the same nutritional conditions, some people gain weight, while others do not. The same food in some people causes a high release of insulin, while in others it does not. Why do different studies on the same topic come to different conclusions? Is this not evidence of the futility of finding general principles of healthy eating?
It should be agreed that despite the general patterns, there are also multiple individual deviations. They are due to the fact that there are genetically and epigenetically determined personality traits that lead to differences in the expression of certain genes, and hence to a possible deficiency/excess of certain receptors, hormones and enzymes. Accordingly, there are a certain number of people who do not have enough enzymes that break down fats, proteins or lactose. In addition, each of us has a certain set of different chronic diseases.
Therefore, if you give several people to eat, for example, ice cream, then for some it can cause a very high level of glucose in the blood, while for others it is quite moderate *. Of course, the more simple carbohydrates we eat, the higher the insulin response will be. But, with the exception of fructose, other carbohydrates cause an unequal rise in blood glucose in different people. There are people who are sensitive to carbohydrates, and there are those who are not. Some people have low nutrient absorption and don't get fat no matter how much food they eat, while others get fat even when they don't eat much.
Likewise, there are people who are sensitive to fat and those who are not. Some people are sensitive to lactose, others to gluten, and others to some other food components. Some people have increased insulin resistance, others have a «leaky gut syndrome», and others have a disturbed balance of the intestinal microflora. Knowing our own individual characteristics can help us choose the most successful diet *.
Genetic differences can affect the efficiency of digestion, the propensity for certain nutrient deficiencies, and the predisposition to obesity and certain diseases (see «Corrective Supplements» section †).
Nevertheless, despite the different intensity of the body's reaction to food products from one individual to another, the direction of this reaction in all of them will be unambiguous. Excess glucose in the blood is equally dangerous for all people. Excess fat also. Meat will certainly produce uric acid. Micronutrient deficiencies will cause health problems for all people. Conversely, food rich in plant polyphenols and fiber will be beneficial for each of us. Thus, despite possible personal differences, general recommendations related to nutrition are fundamentally possible. Although the degree of influence of certain dietary recommendations will vary for different people.
The list of other factors that can affect a person's glucose response to food is extensive, and these factors are not necessarily related to food content. These are, for example, glucose tolerance; level of physical activity; time since last sleep; human chronotype («owls»/«larks»); violation of the circadian rhythm; intestinal permeability; the amount of sodium and the amount of fiber in food; distribution of macronutrient intake by time of day; sequence of food intake (salad → meat → porridge); but especially the type and quantity of intestinal bacteria.
Individual sensitivity to certain foods is a serious circumstance that affects nutritional recommendations. The extreme manifestation of food sensitivity is food allergy, which is caused by an inadequate immune response. While sensitivity is a latent and slow phenomenon, allergies, on the contrary, are obvious and fast.
In 2004, the US Congress passed the Food Allergen Labeling and Consumer Protection Act (FALCPA) *, which identified eight foods as top food allergens: milk, eggs, fish, shellfish, nuts, peanuts, wheat, and soy. At the time of this law, these foods accounted for 90% of all food allergies and serious allergic reactions. Subsequently, sesame was added to this list *.
In 2014, the Food Standards Agency of the United Kingdom compiled its list of food allergens. These included: celery, gluten-containing grains (such as barley and oats), crustaceans (such as shrimp, crabs, and lobsters), eggs, fish, lupins, milk, shellfish (such as mussels and oysters), mustard, peanuts, sesame, soy beans, sulfites (such as sulfur dioxide if the concentration exceeds ten ppm), and tree nuts (such as almonds, hazelnuts, walnuts, brazil nuts, cashews, pecans, pistachios, and macadamia nuts) *.
This, of course, does not mean that all people should stop taking these many beneficial foods. However, this list helps identify foods that may be causing them personal sensitivities and reduce their consumption to a level that won't cause negative effects.
An extremely important role in the individual metabolism of a person is played by the bacterial spectrum of the intestine * *. Clinical studies show that bacterial imbalance can cause insulin resistance, dyslipidemia, and poor glucose control * *. And that a change in eating style can significantly improve the symptoms of metabolic syndrome and reduce carbohydrate sensitivity * *.
In any case, the evidence that our diet is well suited to our personality is health indicators, determined not only by well-being, but also by laboratory tests †. If they go beyond the target, then the diet should be reviewed and adjusted.
Let us agree to consider the best diet as that which has accompanied man for most of his evolutionary history and which, therefore, best suits his genetics and biology. But, as already mentioned, the diet of a person throughout his history has repeatedly changed *. For example, during the transition from herbivorous life on trees to hunting and gathering (~ 2.5-3 million years ago), during the agricultural revolution (~ 10 thousand years ago), in recent times of intensification of agriculture and industrialization of the food industry, and today, during the globalization of the food market *.
It is difficult to say which of these diets should be taken as an example, because there is no understanding of how quickly the diet itself affects the change in human anatomy and physiology *. Archaeologists note the deterioration of anthropometric data of a person and his health with the beginning of the agrarian revolution compared to the Paleolithic era. However, part of their observations may be due to improved life expectancy and safety, due to which the less healthy members of the population did not die, but continued to live and give offspring.
It is difficult to offer a «scientifically based» diet, because our knowledge is constantly deepening, and with it our views on «proper» nutrition are changing. Nutritional guidelines are constantly being reviewed. The problem of instability of the scientific consensus is exacerbated by the fact that many scientific studies are financed by interested financial and industrial corporations, as a result of which their results are often distorted and can even be falsified.
It is difficult to offer a diet that is universal for all people, because each of us has certain genetic characteristics. It is also difficult to offer a food-specific diet because there are limited options for local food choices. Metabolic flexibility, due to which a person adapts to a new diet without noticeable consequences, also does not make it possible to talk about any single correct nutritional formula.
There are many other difficulties in order to be able to offer an ideal diet. Thousands of specialists and completely random people preach on this topic. Millions of dollars worth of popular books have been sold on the subject. On this topic, there are hundreds of the most controversial opinions and theories, the proof and refutation of which will require too much time and facts.
Nevertheless, we have a chance not to drown in a sea of arguments from one side or the other without coming to a definite conclusion. It is enough to analyze the diets of different countries and regions, and compare them with the local incidence rate, to get an idea which of the existing diets is associated with the lowest risk of breast cancer. Thus, we will sum up the planetary natural experiment, where one and a half hundred different nutritional models will be compared.
Such a review has been done previously and is presented separately *. The brief conclusions that follow from it are as follows:
• The risk of breast cancer is directly related to the calorie content of food.
The physiological minimum for adult women of middle age of normal build is 1'600 kcal/day.
The average caloric intake in the 10 countries with the lowest incidence of breast cancer is 2'200 kcal/day.
The average caloric intake in the 10 countries with the highest incidence of breast cancer is 3'300 kcal/day.
• The strongest predictor of diet-related breast cancer risk is the fiber-to-fat ratio. Although fat is not considered a carcinogen or mutagenic compound, it is nonetheless the strongest contributor to the risk of breast cancer of all three essential nutrients.
• Dietary caloric intake and associated obesity appear to be stronger risk factors for cancer than fat intake. However, the share of fat in total energy intake in the 10 countries with the lowest incidence of breast cancer is below 20%.
• The safest caloric balance carbohydrates:proteins:fats, established as a result of analysis of various national diets, is close to the ratio 69:12:19 (in %E).
Weight ratio in food carbohydrates:fats – not less than 2.
The weight ratio in food proteins:fats – not less than 1.
The weight ratio of vegetable proteins to animal proteins is at least 2.
The weight ratio of vegetable fats to animal fats is at least 4.
Weight ratio of fats ω-6:ω-3 – no more than 4.
The daily fiber intake is at least 40 grams.
Daily consumption of simple sugars, including in a latent form – no more than 30 grams.
The consumption of vegetables, fruits and fiber is so critical that it seems that increasing their share in the diet can compensate for the negative role of excess fat.
• Acid load – slightly alkaline.
It may not be the best formula. Perhaps it does not quite meet modern ideas about the ideal diet. Perhaps it does not take into account many personal characteristics. However, of all available, it is associated with the lowest risk of breast cancer.
In defense of the nutritional model proposed below, a table is provided that compares the median averages of the dietary composition of various country groups.
Here, the red10 and green10 are groups of ten countries, respectively, with the highest and lowest incidence of breast cancer among those countries where breast cancer is the predominant type of cancer. The «red10» includes Belgium, France, the Netherlands, Israel, Ireland, Uruguay, New Zealand, Denmark, Great Britain, Finland, and the «green10» includes Turkmenistan, Thailand, Turkey, Mexico, Azerbaijan, India, Uzbekistan, Iran, Belize, Vietnam.
Further, the orange10 is a group of ten countries with the lowest incidence of breast cancer among those countries where breast cancer is not the predominant type of cancer (Congo, Guinea, Nicaragua, Botswana, Zimbabwe, Cambodia, Honduras, Guatemala, Mozambique, Gambia).
And finally, the yellow10 is a group of ten countries with the lowest incidence of all types of cancer in women (Tunisia, Azerbaijan, Uzbekistan, Bangladesh, Sri Lanka, India, Tajikistan, Niger, Yemen, Gambia). So-called healthy diet will be discussed below.
This table clearly shows the differences in eating patterns in each of these selected groups. It is easy to see that the most striking difference between the diets of «unfavorable» and «prosperous» groups exists in the consumption of the most high-calorie foods – animal fats and alcohol. In countries where breast cancer is the predominant type of cancer, the difference in animal fat consumption between countries with the highest and lowest incidence is 1.7 times. In addition, in the «yellow10», compared to the «red10», there is significantly less weight consumption of alcohol (11 times), animal fat (10 times), meat (4.6 times), eggs (3.8 times), milk (3.6 times) and sugar (3 times), but the consumption of cereals is slightly higher (1.6 times). From here it becomes clear which dietary model we should focus on.
An example of a rational diet. To provide the above balances and principles at 2'200 kcal/day, a weekly grocery shopping list might look something like this:
• Whole grains and pseudo-cereals, boiled: buckwheat – 400 g; oatmeal – 200 g; poppy – 50 g; brown rice – 300 g; flax – 100 g; spelled, amaranth, chia, quinoa, false flax, millet – together 400 g. Total – 1.5 kg of dry weight. Whole grain bread – 1'000 g; rye bread – 1'000 g. Optional: wheat bran, linseed cake – 120 g.
• Legumes, boiled: beans, peas – 50 g each; soybeans, lentils, mung beans, chickpeas – 25 g each. Total – 200 g.
• Nuts and oilseeds: walnut – 30 g (15-20 pieces); brazil nuts, pine nuts, almonds, peanuts, cashews, pecans, macadamias, pistachios – together 20 g; sunflower seeds – 40 g; sesame seeds – 30 g, pumpkin, fenugreek, plantain – only 10 g. Total – 140 g.
• Tubers and root crops: potatoes – 500 g; Jerusalem artichoke – 100 g (2 pcs); carrots – 200 g (2 pcs); beets – 350 g (2-3 pieces); parsnip – 30 g (1 pc); turnip – 100 g (1 pc); radish – 100 g (1 pc); selera – 50 g (1 pc); onion – 300 g (3 pcs); garlic – 50 g (1-2 head). In total – about 1.5 kg.
• Vegetables, raw and cooked: white cabbage – 300 g; red cabbage – 300 g; sauerkraut – 100 g; broccoli – 200 g; cauliflower – 300 g; Chinese cabbage – 100 g; pumpkin – 200 g; green beans – 200 g; okra, tomatoes, eggplants, cucumbers, zucchini, sweet peppers – 100 g each. Total – at least 2 kg.
This is the only item on the list whose consumption volumes can be increased uncontrollably. Increasing the consumption of low-calorie foods (vegetables) will mean a reduction in the consumption of high-calorie foods (fats and meat), because the capacity of the stomach is limited. In addition, it will improve the fiber:fat ratio.
• Raw greens: lettuce – 300 g; radicchio, cilantro, spinach, arugula, basil – 100 g; chard, wild garlic, green onions, parsley, dill – 100 g. Total – 0.5 kg.
• Marine plants (algae): 30 g dry weight or 200 g wet weight.
• Mushrooms: 50 g dry weight in the form of mushroom meal (cep, maitake, shiitake).
• Spices: turmeric, pepper, oregano, cinnamon, laurel, coriander, wasabi, nutmeg, cloves, rosemary, etc. Total – 30 g dry weight. Table salt – up to 20 g (1 tablespoon).
• Fruits: lemon – 300 g; avocado – 200 g, unsweetened banana, apples, pomegranate, cherry, kiwi – 200 g each. Total – 1.5 kg.
• Berries: Chinese magnolia vine – 100 g; cranberries – 50 g, honeysuckle, sea buckthorn, viburnum, wild rose, raspberries – 20 g each. Total – 250 g.
• Meat: liver, lean beef, rabbit, lean free range poultry. Total 150 g.
• Fish: fatty herring – 200 g; mackerel – 100 g; cod liver, eel, notothenia, halibut, trout, salmon, pink salmon (alternating choice) – 100 g. Total 400 g.
• Eggs: quail – up to 10 pcs, or, alternatively, chicken – up to 2 pcs.
• Fat-free cottage cheese – 100 g (equivalent to 500 ml of whole milk).
• Drinks: soy, oat or almond yogurt – 400 ml; kvass or other fermented drinks – 300 ml; red dry wine – 1 glass, pomegranate juice – 1'500 ml; aloe juice; green tea, uzvara, alkalizing tonic †.
Vegetable juices are a refined food. But if they are to be taken, they should be in the form of fresh juices, preferably pressed under high pressure; and not in the form of industrial juices, which are poor in vitamins, contain too much added sugar and do not contain plant enzymes.
Fruit juices are a bad idea due to their very high sugar content and low fiber content. The vitamins they contain are too few to justify taking them.
• Sweets: Dried fruits such as figs, dried apricots, prunes, dark raisins or dates – 500 g in total. Although dried fruits, like fruit juices, are full of sugar, they contain many minerals and phytonutrients.
• Additional fats are not included in this list, because. they greatly increase the total calorie content. Although it is better to do without it, the consumption of olive and linseed oil in a ratio of 4: 1 is allowed – a total of 150 g. If cooking requires high-temperature processing, then it is better to take a small amount of saturated fat – butter or coconut oil, but not more than a tablespoon.
Such a fully balanced weekly set of products will correspond to approximately 1.5 kg of food per day, 85% of the total volume of which will be of vegetable origin and will provide acceptable calorie content (2'130 kcal/day), proteins (85 g/day), fats (57 g/day), fiber (70 g/day), cholesterol (215 mg/day), EPA (1 g/day), and DHA (2 g/day). As well as satisfactory ratios of the following nutrients – sodium:potassium (1:2), saturated:unsaturated fats (1:3.7), ω-3:ω-6 (1:1.5), animal:vegetable proteins (1:6), simple:complex carbohydrates (1:2).
The ratio of carbohydrates:proteins:fats in total calories will be 58:17:25 here. Although the balance obtained here falls short of the proposed one and needs further correction, it is close to the target balance. The share of fat in total calories here is close to that of countries with the lowest incidence of breast cancer, the share of carbohydrates is safe *. The level of proteins is, of course, a little high, but the proportion of animal protein is low.
Monitoring weekly food purchases instead of daily monitoring of what we eat allows us to get rid of the tedious routine of monitoring our nutrition and monitor it more comfortably and accurately. However, such a method would require avoiding the consumption of food prepared by third parties from uncontrolled sources.
Pie charts allow you to visualize the composition of a healthy, «anti-cancer diet» in terms of calories and weight of its components. Of course, we do not need to strictly control the grams and units of percent specified here; they were obtained after the analysis of this particular set of products. We are free to choose other products if their set satisfies the requirements established by us above.
Here, whole grains provide almost half of the total calories, but vegetables and fruits account for almost half of the total weight of the recommended diet due to their low energy density. The challenge, however, may be to provide enough nutrients and essential nutrients and minerals without exceeding the recommended maximum daily caloric intake of 2'200 kcal (for a body weight of 65 kg).
To solve it, you can, at a minimum, choose grains with the highest ratio of shell weight to the weight of their contents (wild rice, flax, false flax, chia, quinoa), as well as a sufficient amount of vegetables. It is better to choose vegetables grown in the fields, which are enriched only with natural fertilizers and polymineral additives.
Some of the grain products are high in gluten and gliadin, or other very similar proteins. People who are sensitive to gluten would be better off avoiding foods like wheat, rye, barley, oats, rice, buckwheat, corn, millet, amaranth, and quinoa. Fortunately, there are very few such people.
The addition of bran or flaxseed meal to food also allows you to increase the nutritional value of food without a significant increase in its calorie content. This solution, among other things, allows you to lower the glycemic index of the food you eat, because fiber makes it difficult and slows down the absorption of carbohydrates.
In the proposed weekly set, the share of fat in total calories is 25%, exceeding our planned 20%. Further reductions in fat intake are difficult to implement because the fats that can be reduced further are mostly hidden. Thus, reducing them means reducing the consumption of products containing them.
It is possible, for example, to sacrifice nuts and fatty ocean fish, but this will lead to a decrease in the supply of essential fatty acids, vitamin D, calcium, selenium and iodine, and most likely will require their intake in the form of supplements. In addition, it will reduce the amount of incoming ω-3 fatty acids, which can lead to an imbalance of ω-3:ω-6.
Alternatively, we can increase our intake of carbohydrate foods while proportionally reducing our intake of other foods so as not to increase our overall calorie intake. In any case, the addition of pure fats (vegetable oils, butter, chocolate, lard, etc.) to food will dramatically increase the fat portion of the daily calorie content.
This diet is not vegan, as it includes fish, as well as small amounts of eggs and lean meats. This is guaranteed to provide the body with nutrients that are difficult or impossible to obtain from plant foods. These are, for example, vitamins – А, В6, В12, D, F; amino acids – creatine, carnosine, taurine; coenzyme Q10 and conjugated linoleic acid. Thus, there is no need to take them in supplement form.
Vegans could compensate for cutting out meat by increasing their consumption of legumes, mushroom flour, nuts, and seeds by 10% to keep their protein intake at the right level. However, there is no particular need for such a desire, because there is more than enough protein in the proposed diet. Even if animal protein sources (eggs, cottage cheese, meat and fish) are completely excluded from this list, the daily dose of protein from other sources will still be significantly higher than the WHO recommended daily protein intake for an adult (40 g). And the amino acid profile of the consumed plant foods will ensure that we receive a complete set of amino acids in sufficient volume.
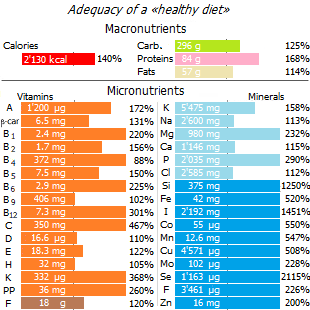
The proposed low risk diet (healthy diet) is close to the diet of the blue10, that is, the group of ten countries in the world that are most prosperous in terms of breast cancer (Gambia, Nepal, Bangladesh, Guinea, Lesotho, Tajikistan, Zambia, Botswana, Mozambique, Uganda *). The average diet of this ten can be taken as a guideline. Or you can try to improve it by increasing those foods that are associated with risk reduction * *. Our cancer-fighting diet, for example, is increased in legumes, nuts and oilseeds, vegetables and seaweed; reduced proportion of alcohol, milk and total fats; and shifted animal protein intake from red meat to ocean fish.
Systematic reviews of the best-known dietary patterns also conclude that diets that protect against breast cancer are necessarily rich in vegetables, fruits, and fish, while diets associated with an increased risk of breast cancer contain saturated fat, alcohol, red and processed meat * * *.
Analysis of the composition of the proposed anti-cancer diet shows its usefulness. On many counts, it provides micronutrient redundancy compared to recommended daily doses. However, many of the suggested «weekly food list» products may not be suitable for some people due to individual sensitivity/intolerance. People with other diseases, including autoimmune diseases, will also have to toughen their choices. Again, specialized programs can be of great help in ensuring the usefulness of your diet. Each of us, based on our preferences and individual characteristics, can make a diet that is more suitable for ourselves, guided by the principles outlined above.
A preliminary estimate suggests that switching from a «Western» to a «healthy» diet would reduce the risk of breast cancer by a third *, and reduce the relative risk of overall mortality and recurrence in patients with already diagnosed breast cancer by 1.6-3.7 times * * * *.
Popular publications are brimming with superfood recommendations and with healthy recipes. However, the typical expressions "this product needs to be eaten more" are fundamentally wrong. Because for the practical implementation of a complete and balanced diet, it is important to know not only which products are best to choose, but also their quantity and ratio. The above weekly list of easily accessible foods is such an attempt.
The analysis shows that although the diet of the proposed «healthy diet» remains excessive in terms of calories and fat content, it almost completely provides the recommended intake of vitamins and minerals, and also satisfactorily ensures their balance. Of course, this proposal is not perfect, and could be greatly improved, but even a primitive plan is better than no plan at all.
The benefits of the proposed diet compared to some other known diets can be seen in the comparison table given here *. The proportion of total carbohydrates in it is higher than in the «Mediterranean» diet, but lower than in the low-fat diet; the proportion of fat and protein is higher than in a low-fat diet, but lower than in all others.
The glycemic load of such a diet is lower than that of a modern diet due to the reduction in simple carbohydrates, although probably higher than that of a high-fat diet. However, it can be brought to the level of the «Paleolithic» diet due to more frequent meals, i.e. such a regime of its consumption, which is characteristic of all wild primates.
The calorie content of the «healthy diet» is close to Ornish's vegan diet. It is lower than that of the «Mediterranean» and «Paleolithic» diets, because the physical activity of modern man is low compared to the Paleolithic. The acid load is also quite low, and the intake of fiber and micronutrients is satisfactory.
It is noticeable that other popular diets are inferior to it in most indicators. The dietary structure of such a diet is intermediate between the «Mediterranean» and low-fat diets of rural areas of Asia, Africa and Japan, where there are the lowest rates of breast cancer. Worse than others here are the low-carb Atkins diet, and especially the modern «Western» diet.
The proposed «healthy», aka «anti-cancer» model of nutrition is in good harmony with modern scientific ideas about a healthy diet. In 2020, the US Dietary Guidelines Advisory Committee conducted a systematic review of 153 feature articles over the past 20 years to examine the relationship between dietary patterns consumed and all-cause mortality *. The findings presented in this report are fundamentally consistent with the findings outlined above.
In general, dietary patterns that emphasize a higher intake of vegetables, legumes, fruits, nuts, whole grains, fish, lean meat or poultry, and unsaturated fats compared to saturated fats have been associated with a reduced risk of all-cause mortality.
Of the eating patterns that included animal products, protective associations were generally observed with relatively less consumption of red and processed meats.
A reduction in the risk of all-cause mortality has also been observed in several studies that have examined diets without animal products, such as those described as vegetarian, vegan, or index-based «plant-based» diets.
The inclusion of white:red meat ratios, type and amount of dairy products, and refined carbohydrates and sweets as elements of these patterns was less consistent across the evidence.
Dietary regimens that included the following and tended to show a reduced risk of all-cause mortality:
- higher consumption of white meat compared to red or processed meat,
- low-fat dairy products compared to high-fat dairy products,
- lower compared to higher consumption of refined carbohydrates and sweets.
Although nearly all were prospective cohort studies, most were adjusted for major confounding factors.
It is good that a modern person has both a sufficient choice of products and a mind in order to provide himself with a healthy, complete diet. Too bad people don't usually do this.