Health Strategy.


The first symptoms of breast cancer are usually tenderness, swelling, areas of hardened tissue in the breast (A), or a lump in the breast or armpit (B).
Most seals are not cancerous, but each should be carefully checked by a specialist. Pain in the armpits or breast that does not depend on monthly cycles can be another early symptom.


Other outwardly manifest symptoms may include:





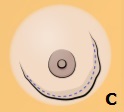
• swelling, change in size or shape of the breast (C);
• covering of the breast with ripples, depressions or scales (D);
• lumpiness or redness of the breast skin (E);
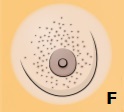
• orange peel texture (F);
• ulcer on the nipple (G);
• sunken or deformed nipple (H);
• displacement of the center of the nipple (J);
• roughness of the nipple (K);
• discharge from the nipple that does not look like milk, including blood (L). As a rule, yellowish or greenish discharge is benign, in contrast to tea-colored or colorless discharge; but this is not necessarily the case.
At the very early stage of the disease, it is almost impossible to distinguish the onset of a tumor from other disease states. All of the above symptoms are characteristic of an already sufficiently developed disease, when a tumor can be diagnosed.
However, long before the cancer is detected by the test, women may experience the following symptoms of early breast cancer:
• mild pain, swelling and irritability of the breast; enlargement of skin pores; inconvenience from a bra, a feeling of «interfering» breasts;
• swelling, soreness or hardening of the lymph nodes; slight pain in the shoulder blade; slight swelling and numbness of the hand;
• headaches or dizziness; chronic fatigue, shortness of breath, weakness and/or drowsiness; leg cramps;
• abnormal body temperature, chills, night sweats; offensive body odor; other symptoms of latent inflammation;
• non-healing small wounds; herpes; frequent colds; other manifestations of reduced immunity;
• poor falling asleep and awakening; insomnia; excruciatingly heavy, poor and/or interrupted sleep.
The diagnosis of fibrocystic mastopathy, and even more so a benign tumor, should already be a serious reason to think about a possible malignant transformation that has begun. The process of cancer development can be too hidden and disguised. And the transition from pre-cancerous to cancerous can be very quick and unexpected. And, unfortunately, it is very easy to miss this turning point.
Diagnostic evaluations of breast cancer usually include the following procedures.
The blood test will allow medical staff to assess the patient's health status and develop the best treatment plan.
A common blood count is taken on an empty stomach and is used to measure the amount of blood (or the number of blood cells circulating in the bloodstream). In particular, the blood sample measures the level of blood cells – red blood cells (carrying oxygen throughout the body), white blood cells (fighting infection) and platelets (blood clotting). Their number may vary in tumor conditions.
A complete blood count also measures hemoglobin (the protein in red blood cells that carry oxygen) and hematocrit (the ratio of red blood cells to plasma), as well as many other blood chemistry indicators that allow one to draw a conclusion about the work of the patient's internal organs.
An analysis of nipple discharge for blood and abnormal cells may also be done if necessary.
External examination and palpation are the most accessible and free diagnostic methods *. Given the increasing incidence of breast cancer, every woman should be able and regularly check the condition of her breasts by examining and probing for the early symptoms of cancer listed above. At a minimum, this should be done every week after the end of menstruation, and in the absence of menstruation, every month on the same day. The slightest suspicion gives rise to an unscheduled visit to your doctor, which cannot be postponed. The procedure for self-examination and palpation will be described below†.
Palpation (examination by feeling tissue) allows you to detect suspicious formations, as well as their size, shape and consistency. However, palpation does not allow to detect a tumor at the earliest stages of its development, and is insufficient for any definite conclusions; therefore requires more in-depth research.
Clinical breast examination may be performed by a trained healthcare professional during a routine. One study reported that almost 9% of cancer patients were diagnosed with only one clinical breast examination, and if it had not been performed, these cases would not have been diagnosed in time *.
X-ray studies. There are several types of chest x-rays.
Mammography is a low-radiation X-ray examination used to detect and diagnose breast cancer tumors that are too small or too deep to be detected by an external examination of the breast. Modern 3D gamma machines are able to detect tumors that can be obscured by dense tissue on conventional 2D mammograms.
Category |
Description |
0 |
Incomplete study. Further investigation required. |
1 |
Negative conclusion (no deviations were found). Follow-up is routine screening. |
2 |
Benign changes. Should be considered when evaluating future mammograms. |
3 |
Probably benign changes, but not necessarily benign. More frequent follow-ups are recommended to check for any changes. |
4 |
Suspicious abnormality. 4A: low level of suspicion of malignancy (~ 2%). 4B: intermediate suspicion of malignancy (~ 10%). 4C: moderately suspicious (~ 50%), but changes are not classic for malignant tumors. A biopsy is usually recommended. |
5 |
Changes characteristic of cancer. Biopsy required. |
6 |
Cancer confirmed by previous biopsy. Follow-up depends on the purpose of the mammogram. |
To standardize the presentation of mammography results, the BI-RADS * classification system has been created.
In recent years, the need for mammography has been reconsidered due to the dangers of ionizing radiation, possible diagnostic errors, and the inconclusiveness of its impact on reducing mortality * *. Cases of breast cancer in women aged 40-50 years without an increased risk are relatively rare, and false positive results are frequent *. However, mammography is still the main diagnostic procedure for breast cancer.
Mammography can detect breast cancer in its early stages. But since mammograms reveal a cancer of an average size of 13 mm, annual regular examination and palpation remains important. However, neither mammography nor palpation are reliable methods for detecting cancer.
Mammography may suggest cancer or a precancerous condition, but it also often reveals calcified areas in the breast that occur for various reasons. Tumors found on mammograms are most often benign. Many of the small tumors found on a mammogram may never progress and it is estimated that one in five of them may disappear on their own without being detected * * *.
Without screening, one third of all invasive breast cancers in the 50-69 age group would not be detected during the patient's lifetime and would not cause her death. This level of overdiagnosis is much higher than previously thought *. It is estimated that for every life saved by a mammogram, between 2 and 10 women are overdiagnosed *, leading to them being diagnosed with breast cancer and receiving health-threatening treatment that may not actually be necessary. The risk to life is actually not so much the size of the tumor detected by mammography, but the rate of its growth and the ability to metastasize.
The rate of false-positive results especially increases in patients older than 40 years of age. Therefore, abnormalities detected by mammography require additional biopsy to establish a definitive diagnosis *.
Mammography is not prescribed for women under 35 without convincing reasons.
Aiming radiographs allow you to increase the x-ray image by 1.5-2 times, which allows you to study in more detail certain areas of the breast that are poorly visible on mammography or fluorography.
Three-dimensional mammography (3D-mammography) is the most modern method of mammography. Here, several images taken from different angles are combined to create a three-dimensional image *. This technology is expected to be able to detect more tumors than conventional mammography and reduce false positives *. Currently, 3D mammography has not yet been introduced into widespread practice.
Tomography is a minimally traumatic procedure for obtaining cross-sectional images of the breast that allow differentiation between normal and tumor tissue, revealing the sites of initial tumors and metastases. Tomography is used both as an addition to mammography and as an alternative *.
Computed tomography (CT) uses a rotating X-ray beam to create detailed computerized images of the breast, allowing you to identify tissue abnormalities and their exact location. CT can detect objects as small as 3 millimeters, and the use of contrast agents allows you to see cancer cells that consume more glucose than normal cells, as well as assess the intensity of its consumption.
Magnetic resonance imaging (MRI) provides greater contrast in the soft tissues of the body than computed tomography and is often used to image the brain, spine, muscles, connective tissue, and the inside of bones. Unlike CT, MRI does not use ionizing radiation.
Compared to mammography, MRI is independent of breast density and has advantages in detecting occult primary breast cancer, axillary nodal metastasis, residual tumors after neoadjuvant chemotherapy, or other small tumors *. Modern MRI scanners can measure tissues as small as 0.5 mm3, with a detection rate of 37-100% *. Due to its high sensitivity, MRI may be useful for definitive follow-up in high-risk groups when mammography results are still normal. At the same time, MRI gives a high percentage of false-positive results.
Positron emission tomography (PET) is another modern technology that uses high-energy, short-lived isotopes. PET can identify areas of increased metabolism, more accurately identifying the location of a rapidly growing tumor and distinguishing it from other abnormalities. PET makes it possible to detect metabolic changes in dubious nodes long before the onset of changes noticeable by other means. However, PET can sometimes give false results too. Even though PET uses stronger radiation than CT, patient exposure remains very low due to its short duration.
Scintimammography is another gamma imaging technology that allows you to refine and detail abnormalities detected using mammography *. It is used as an adjunct to mammography and may be useful in cases where the breast condition is difficult to assess with conventional mammography, for example due to high mammographic density, implants, or existing non-malignant disease *.
Here, a gamma camera captures the radiation of a radioactive substance previously injected into the patient and accumulated in the mammary gland *. This technology allows you to get a result with a much lower number of false conclusions than MRI *.
Bone scintigraphy is a radionuclide diagnostic that uses radioisotopes that are deposited on the bone tissue, concentrating at the sites of metastases and other bone diseases. A bone scan can reveal whether breast cancer has spread to the bone. Scans can detect cancer cells, evaluate bone fractures, and monitor for other bone conditions such as infections and arthritis.
Ultrasound examination allows you to visually detect the slightest deviations in the density of the breast and determine whether the lump is a cyst (a sac containing fluid) or a solid tumor. Ultrasound can also be used to accurately determine the position of a tumor, such as for sampling during a biopsy procedure. The best results are obtained when the mammary gland has sufficient acoustic density to allow sound to pass through.
Ultrasound is a fairly safe procedure. Although it does not give an exhaustive picture of the changes occurring in the female breast, it can complement X-ray studies well.
Radiothermometry (thermography) measures the difference in temperature in different tissues of the body and allows visualization of the tumor due to its higher temperature compared to healthy tissue. This diagnosis allows detection of lesions in mammographically dense tissue, however, it is not an effective alternative to screening mammograms for breast cancer *, and is used as an additional method.
Miraluma displays high-quality images of malignant growths among the dense, fibrous breast tissue and helps to detect malignant tumors that may have missed other tests, as well as tumors at an early stage.
A promising direction in the development of non-traumatic diagnostics is the visualization of the redox activity of tissue * *. It makes it possible to detect malignant transformations at the earliest stages, when a tumor cannot be detected even with high-resolution MRI, since metabolic disorders can be signs of cancer that occur and are diagnosed earlier than detectable histological changes *. But such diagnostics is not yet used in clinics.
A biopsy is the most reliable way to examine a patient's tissue. Today, this is the only reliable way to determine whether a tumor is benign or malignant. During a biopsy, a sample of tissue or fluid from the body is taken and the cells are then examined under a microscope to determine if they are malignant. If the cells are identified as cancerous, a biopsy can help determine if the cancer started at the biopsy site or if it started elsewhere in the body and only then spread to the biopsy site.
Some biopsies are done with an endoscope, others with imaging techniques such as ultrasound, computed tomography (CT), or magnetic resonance imaging (MRI). In some cases, biopsies are performed during surgery, allowing tissue to be harvested from deep within the body. A lymph node biopsy can determine if breast cancer has spread to the lymph nodes under the arm.
Although it is impossible to be sure of the malignant nature of the tumor without a biopsy, the procedure itself is traumatic. This means that it causes local inflammation, and inflammation contributes to malignant transformations. Thus, in a patient with a benign tumor, the chance of getting a malignant tumor over time increases, despite the favorable results of the biopsy.
In addition, a biopsy violates the physical barrier of the tumor from external tissues, because in order to extract a sample of tumor tissue, one has to pierce the so-called. basement membrane – a dense protein film that surrounds the tumor. And if the tumor is really malignant, then cancer cells get a free passage for metastasis. As Dr. Thomas Seyfried poignantly described the procedure, "we make a hole in the hive to look at the honey, but a swarm of angry bees fly out of it."
The molecular profile of a tumor examines a sample of a primary tumor, a metastatic tumor, or a recurrent breast tumor, often taken as part of a biopsy or other surgery. Here, various enzymes, proteins, and genes are analyzed to determine which drug therapies may be most effective.
Biopsy together with cell receptor analysis allows to determine the subtype of cancer (ductal or lobular) *; conduct a satisfactory histological assessment of the tumor (the degree of deviation of cancer cells from normal) *, as well as evaluate the molecular characteristics of cells (ER, PR, HER2) *. The data obtained from the biopsy is very important for planning the treatment protocol.
Liquid biopsies are a term for multifunctional biomarkers circulating in peripheral blood and other bodily fluids. Modern highly sensitive methods can detect tumor cells or tumor DNA circulating in the blood * and predict the risk of cancer metastasis *. In addition, this type of research allows finding ways to overcome drug resistance, and to find out if the molecular profile of the tumor changes during treatment *.
Liquid biopsies are a promising non-invasive alternative to tissue biopsy, but this promising method has not yet been used in clinical practice in breast cancer * *.
Genomic research examines a tumor at the genetic level to detect changes in DNA that lead to cancer growth. The American Society of Breast Surgeons recommends that all cancer patients undergo multi-gene panel testing to assess their inherited risk of developing breast cancer *. By identifying mutations occurring in the genome of a cancer cell, it is possible to better understand what caused the tumor, and based on these results, develop an individual treatment. It will also help the patient's relatives understand their genetic risk of developing cancer and take preventive measures to reduce their own risk of developing cancer.
Mammaprint and Blueprint are used to decode the unique properties of a breast tumor and allow the development of a treatment plan specific to the individual needs of the study patient with stage I or II disease. Mammaprint examines the expression levels of 70 genes in a tumor *, and Blueprint examines 21 genes *, and the results of the studies categorize patients as high and low risk *.
The Oncotype DX (otherwise known as the 21-gene test) is used to find out if chemotherapy can benefit patients with early-stage breast cancer, as well as to assess the likelihood of a recurrence of the disease. However, to reliably determine the actual markers of cancer cells, their molecular profile should also be studied.
Breast autopsy of middle-aged women (20-54 years) who died of causes not related to cancer shows that 7% of them had atypical hyperplasia, and 20% had hidden malignancies: 18% in situ and 2% aggressive; most of them measured less than 5 mm *. Diagnostics could not clearly identify them during the life of these people. Of the 80 women examined postmortem without malignant and atypical lesions, only 5 had a diagnosis of various benign breast diseases during their lifetime, that is, 1 out of 16.
These figures indicate that in most cases the disease eludes the earliest diagnosis. And that by the time modern diagnostics give grounds for a biopsy, the tumor can reach an unacceptably large size. However, this sad picture should not cause panic. At the earliest stages of trouble, all processes are reversible. If every fourth woman wears hidden tumors, then this threat should not be dismissed. It’s just worth leading a lifestyle that would not allow them to form, and the development of existing, yet undiagnosed tumors, would reverse. Act as if the tumor has already been diagnosed.
Not all patients are assigned the same examinations before starting treatment.
Assigned examinations |
To whom are assigned |
Common blood analysis |
All |
Complete biochemical blood test |
All |
CT chest with contrast |
All |
CT/MRI of the abdomen and pelvis with contrast |
All |
Bone scintigraphy |
All |
Biopsy |
All |
Hormone receptor analysis |
All |
Determination of HER2 status |
All |
MRI of the spine with contrast |
For specific symptoms |
MRI of the brain with contrast |
For specific symptoms |
X-ray of bones |
For specific symptoms |
Prospects for diagnosis. Every year more and more new diagnostic methods are being developed. They claim that they will be able to detect ever smaller tumors, i.e. at an ever earlier stage. Indeed, they allow you to more accurately and in more detail see the current picture of the disease. But, taking into account the fact that many years pass before tumors form as a special formation, all these methods actually still refer not to «early», but to «late» diagnosis.
Diagnostically it is difficult to detect the line that separates the tumor from the abnormal changes in the breast tissue that precede it. In addition, we actually need to diagnose not an already existing tumor, but precancerous conditions, pathologies that are guaranteed (and not supposedly) to lead to cancer. This will allow us to avoid cancer, and not start its treatment at an early stage.
Therefore, it would be better, without waiting for the worst outcome, to treat any painful condition of the breast as a precancerous condition that should be persistently corrected, and preferably by non-drug means.