Health Strategy.
• Epigenetic modulation normalizes gene expression by silencing oncogenes and activating antitumor genes.
• Metabolic correction suppresses glycolysis and promotes tissue oxygenation.
• Anti-inflammatory therapy alleviates signal stress on breast cells and counteracts both general and local latent inflammation, which is the central process of tumor development.
• Immune modulation normalizes the immune system and promotes the natural destruction of cancer cells.
• Gut health improves immunity, reduces estrogen load and blood toxicity, increases vitamin production, and improves overall health.
• Acid-base and electrolyte modulation reduces acid stress in tissues, restores the body's alkaline buffers and electrolyte balance.
• Diet and exercise are the most influential and most easily modifiable risk factors for breast cancer.
• Additives of missing vitamins and elements allow to ensure the normal functioning of all body systems.
• Increased overall vitality, detoxification and organ support strengthens the general condition of the body and increases its resistance against all diseases.
• Hormonal modulation allows you to restore the disturbed hormonal balance, reduce the estrogen load and normalize the harmonious functioning of the main hormones.
• Normalization of breast tissue can reduce the risk of cancer and worsen the conditions for its development.
• Suppression of cancer cells inhibits the growth and malignancy of the tumor.
In addition to medicine called official, orthodox, or traditional, there is medicine called non-traditional. Non-traditional therapies are any medical system, practice, or product that is not normally used in standard treatment protocols.
Alternative medicine is divided into complementary, alternative and integrative.
The practice of orthodox medicine is evidence-based. The methods or treatments she uses are pre-tested in clinical trials and provide demonstrable results in the course of treatment. Complementary medicine treatments are based on a scientific approach and evidence based principle and are used as a complement to conventional medicine. Alternative medicine therapies are most often based on contraversional functional hypotheses, and are used instead of conventional medicine. And, finally, integrative medicine is a synthesis of traditional and non-traditional (naturopathic) medicine in the part that has proven its practical effectiveness.
In orthodox medicine, new ideas and tools go through a long, regulated, and costly journey of proving their effectiveness, culminating in clinical trials. And for this reason, the beginning of their application may be years and decades behind the moment of their birth.
The traditional «gold standard» (scalpel, poison and radiation) is still the main tool in the treatment of breast cancer. At the same time, there are many drugs with proven efficacy that are not accepted in clinical practice, but which could also be useful in various ways. Some of them are common foodstuffs; and some have long been used in other areas of medicine, and therefore do not require proof of their safety.
Choice of treatment protocol. As a rule, patients turn to traditional treatment practices practiced in specialized medical institutions. When developing a treatment protocol, doctors will take into account: the stage of cancer development and its aggressiveness; age and menopausal status; the status of cancer hormone receptors and HER2; the general state of health and the ability of the patient to endure this or that treatment; the possibility of surgery and many other individual features. Sometimes there is a refusal of traditional methods of treatment: either on the part of the patient, or on the part of doctors who believe that the treatment will not improve the initial condition.
In many cases, patients sometimes resort to alternative therapies, however wild and unproven they may be. Most people seek alternative therapies not because they are stupid or uneducated; not because they don't trust doctors; and not because they are irresponsible or gullible. Most often this happens because they do not see the success of the treatment offered to them by doctors. Or they see that for doctors the focus is on the tumor, and not on the health of the patient. For many, the cost of standard treatment protocols also plays an important role.
Unfortunately, many proposals addressed to these unfortunate people have no scientific basis. These are well-known methods of treatment with urine, vodka with oil, highly toxic substances outside the clinic, and other equally insane and dangerous adventures that can give nothing but harm. We will focus only on those approaches available to us that have at least some scientific basis and positive practice.
The popular literature provides many useful but often unsystematized facts about alternative or complementary cancer therapies. The integrated approach presented below is an attempt to consider and bring together therapeutic interventions aimed at key factors in the development of breast cancer.
All of the manipulations and natural substances listed below have shown a certain effect in preclinical experiments and some clinical trials. They can be used both for preventive purposes and at any stage of treatment, as well as in the post-therapeutic period.
Complexity of therapy. It would be natural to assume that, since cancer is a multifactorial process, the approach to its treatment should be complex. Attempts to find the cherished patented molecule are wrong in principle. There is not and cannot be any supersubstance or manipulation that can directly rid a person of cancer. But there are many sound recommendations, all of which reduce the risk of cancer initiation, development and metastasis, increase the effectiveness of anti-cancer therapy and maintain breast health.
In other words, there is no cure for cancer, but there is a treatment that can prolong the patient's life, ideally to death from old age or other causes, and in some cases even reverse the disease.
There are many therapeutic directions that have their own specific purpose. However, no monotherapy can boast of outstanding success. As already mentioned, cancer cells exhibit a high degree of resilience and adaptability to lethal conditions, using complex survival strategies in critical situations, including alternative signaling pathways and genomic modifications.
Even modern combined therapies used in the clinic target only a few therapeutic targets, leaving cancer cells with a wide operating room to maneuver. It makes no sense to put guards at the gate if there are gaping holes in the fence.
It is necessary to ensure the widest and densest possible front of attack on cancer through the use of as many therapeutic targets as possible. A multi-targeted approach can more fully prevent various conditions and opportunities for cancer. At the same time, one should strive for the minimum number of drugs used for therapy – if possible, natural and/or over-the-counter *. The fact that each of them has little effect on its own should not stop us. The sum of small efforts can produce far greater results than one big effort.
Collaboration between doctor
Often the doctor directively prescribes a treatment protocol, without wasting time explaining it and not seeing the need for it. And half of the patients resort to some form of self-addition of the prescribed treatment * * * without informing the attending physician about it. And not always what they use has a reasonable justification, is compatible with the prescribed treatment and is capable of bringing at least some benefit instead of harm. At the same time, only an experienced specialist knows what can be allowed in this situation, and what should not be allowed in any case.
It is unlikely that the attending physician will tolerate the secret initiative of the patient, and it is not difficult to understand him. When planning a treatment protocol, the doctor does not expect its hidden distortions, because they can worsen the final result. Thus, the responsibility for any addition to the prescribed protocol falls on the shoulders of the patient himself.
On the other hand, doctors are not inclined to add anything out of the ordinary to standard treatment protocols. First, fearing their unforeseen interactions. Secondly, even being free in the choice of protocols, the doctor remains not free to use supplements that are not officially approved due to the lack of a convincing evidence base.
Indeed, while all of the agents discussed below have successfully completed preclinical studies, and some have long been used in other diseases, many of them have not been clinically tested in cancer. And they will probably never be clinically tested or in demand by the existing medical business due to lack of commercial interest. This means that they have little chance of passing clinical trials and thus being approved for use.
Warning. All the facts presented in this work should be evaluated critically. It is always worth remembering the side effects and contraindications of each remedy, their possible interactions with each other and with the prescribed main therapeutic agents.
It is known that in certain situations the use of additional agents can increase the toxicity of therapeutic drugs or, conversely, reduce their effectiveness *. For example, that St. John's wort (Hypericum perforatum), which is missing in our review, reduces the effectiveness of most drugs *. Thus, extreme caution is required in the application of additional funds to the main therapy.
To assess the credibility of studies, it is worth paying attention to the conditions under which the anticancer effect of a particular substance was found: in vitro, in experiments on living organisms (in vivo), or in clinical studies. In vitro conditions (oxygen saturation, acidity, nutritional availability, influence of the microenvironment, etc.) may differ significantly from those observed in a tumor. Therefore, in vitro results may differ significantly from in vivo results, and only suggest a possible effect, but do not prove it in any way.
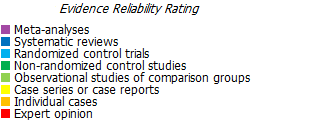
Observational studies are less conclusive than manipulative studies, and animal studies are less conclusive than human studies. Animal studies usually use genetically modified mice, whose metabolism is not identical to humans, so even the expressive effects of a particular substance are rather difficult to scale to humans.
Therefore, studies in vitro have the lowest degree of evidence, in vivo – slightly higher, and the highest degree are randomized double-blind or cross-blind, placebo-controlled studies in patients conducted in several independent research centers with a large number of subjects.
Unfortunately, for many promising substances that have shown their effectiveness outside the body, clinical trials have either not been conducted, or their results are not available. And some that have successfully proven their effectiveness in clinical trials have not been approved for practical use. This is especially true for cheap or natural (i.e. obviously non-patentable) molecules. If something is curative but cannot generate high profits, then it has little chance of finding funding for research. Therefore, often, as is the case in court proceedings, one has to rely not on direct evidence, but on assumptions that are based on a body of circumstantial evidence.
Malignant transformations occur as a result of a high oncogenic load caused by a variety of carcinogenic factors. They begin and are accompanied by characteristic metabolic disturbances, which are likely to remain in place even after therapeutic interventions, thus creating a high chance of recurrence of the disease *. Therefore, it is not enough to conduct a standard course of treatment. Do not prematurely rejoice at the reduction in the size of the primary tumor. The disease has a high chance of reappearing, if the conditions due to which it arose and developed are not changed.