Health Strategy.
Tumors are still an intriguing mystery. They may grow rapidly or slowly, remain without growth, or even regress *. They may not give noticeable metastases for many years, or they may metastasize already at the earliest stages. They can not only spontaneously appear, but sometimes spontaneously disappear without certain understandable reasons * *. It is possible that a person can experience several such small episodes in his entire life without even knowing about them. The so-called «primary tumors» can actually be caused by migrating cancer cells with an unknown initial localization *, while the immune system has already managed to deal with the real primary tumor focus. Further study of tumors will present us with many more interesting surprises.
Currently, scientific opinion tends to be that cancer is a preventable disease *. Single or multiple cells capable of developing a tumor are believed to be present in each of us, but not all of us survive to cancer. Tumor-forming cells spontaneously appear during life, accumulate or disappear due to the reaction of immune cells – quickly or very slowly. As autopsy shows, microscopic tumor foci can be found in more than a third of women 40-50 years old, but they are usually dormant, asymptomatic and difficult to modern diagnosis *. However, in some women, malignant cells are stimulated to grow, become active, and develop into a disease.
Although the likelihood of developing a tumor is driven by a combination of clarified and as yet unexplained causes and biological mechanisms, it is clear that risk factors significantly increase its risk. Cancer Treatment Centers of America has identified some of the most significant known risk factors for breast cancer *, which will be discussed below.
Sex. Breast cancer is 100 times more common in women than in men.
Age. The incidence of any subtype of breast cancer varies with age, as shown in the figure.
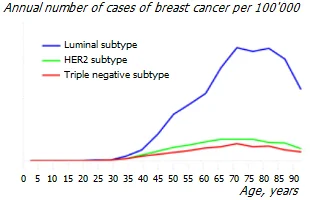
Breast cancer is on average more commonly diagnosed in older women. Only about 10-15% of breast cancers occur in women younger than 45 *. But this pattern may differ for different races or ethnic groups. So, in white women, the luminal subtype is significantly superior to other subtypes, and in black, Hispanic and Asian women, its superiority is less pronounced *.
At the same time, the susceptibility of the mammary gland to carcinogens is highest before the age of 20 years *. It is generally accepted that from the moment of the birth of a malignant tumor to its detection, an average of 15-16 years passes. Therefore, the peak incidence at the age of 65, which we see on the graph, apparently has a peak of initialization at the age of about 50 years. And, most likely, by this age, women already have significant problems with the mammary gland, which in the end end so tragically.
Genetics. Gene analysis reveals the presence of potential genetic problems, especially in families where there is a history of breast cancer.
Women who carry the BRCA1 and BRCA2 genes, compared with the population average, have a 10 times higher risk of developing breast cancer, ovarian cancer, or both *. These genes can be inherited. Mutations in several genes, including CDH1, PTEN, TP53, CHEK2, and ATM, are also associated with an increased risk of developing breast cancer *. In addition to these, other rare mutations, or combinations of them, may make some women more susceptible to developing breast cancer.
Any woman can have a DNA test to look for genetic mutations that increase the risk of breast cancer. However, regardless of whether a woman has a favorable heredity or not, genetic mutations that occur under the influence of specific environmental risk factors are the cause of a much higher number of cancers *.
Indeed, studies of identical twins have shown that genes are not a binding factor in most chronic diseases. For example, concordance (similarity) between identical twins for breast cancer is only about 20% *. Only 5-10% of all cancer cases are caused by the manifestation of genetic defects, and the rest are caused by changeable environmental factors. Thus, 90-95% of cancer cases, like other most common chronic diseases, are caused by non-genetic factors, mainly habitat, lifestyle and diet.
As Max Lugavere so eloquently remarked, "genes only power the trunk, but it is our lifestyle that pulls the trigger."
Infections. The most significant infectious risk factors are considered human papillomavirus (HPV), human cytomegalovirus (HCMV), Epstein-Barr virus (EBV), polyomavirus (SV40), John Cunningham virus (JCV), bovine leukemia virus (BLV), human breast tumor virus (HMTV) *.
However, not only the infections themselves, but the fight against them with antibiotics can also increase the risk of breast cancer by affecting the healthy intestinal microflora.
Chronic inflammation. Inflammation is the central site of the tumor process, and chronic system inflammation is also the main cause of almost all degenerative diseases. Inflammation can be caused by a wide variety of factors, which are discussed in more detail in the «Anti-Inflammatory Therapy» section †.
Body mass. Obesity to some extent increases the risk of almost all diseases. Breast cancer is no exception *. Fat cells can be considered as endocrine cells. Because they produce estrogen, women with excess body fat have higher levels of estrogen in their blood. And high unbalanced estrogen levels increase the risk of developing breast cancer. Weight gain during adulthood and excess fat around the waist can also play a role.
Postmenopausal women with excessive deposits of fat in the abdomen («belly») fall into the zone of particular risk *. The fact is that visceral fat (accumulating around the internal organs) is metabolically more active than subcutaneous fat, for this reason it poses a greater threat to health. Excessive visceral adiposity has been linked not only to an increased risk of breast cancer * but also to metabolic syndrome (MS), and the chronic inflammation that accompanies MS further increases this risk *.
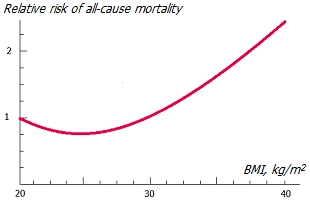
Excess adipose tissue increases the expression of not only estrogen, but also fatty acid binding protein (FABP4). Entering the bloodstream and reaching the mammary gland, FABP4 stimulates the growth of a breast tumor *. In addition, adipose tissue produces cytokines, increasing levels of chronic inflammation. Which, in turn, increases the risk of many degenerative diseases, including cancer.
Obesity not only increases the risk of cancer, but is also a strong predictor of poor breast cancer outcomes, especially in postmenopausal women. In particular, tumors in obese patients are more likely to cause distant metastases *.
Certain disease conditions, such as diabetes * *, high blood pressure *, high cholesterol * or fasting glucose * *, may further increase the risk among obese women. Even non-fat-related body mass gain is associated with a 30% increased risk of breast cancer recurrence and an almost 50% increased risk of death despite optimal treatment *.
Interestingly, being thin during adolescence and being overweight later in life also increases cancer risk, while shedding fat in adolescence between ages 18 and 20 does the opposite *.
Some indicators of the body, although associated with the risk of breast cancer, nevertheless, are not the cause of the disease. For example, the volumetric density of bone tissue in patients with ER-positive cancer is higher than usual * *, which may be as much a consequence of high estrogen levels as the cancer itself *.
Physiological changes in the breast. Certain benign (noncancerous) or precancerous breast conditions can markedly increase the risk of breast cancer. Examples are atypical mammary duct hyperplasia or non-invasive lobular carcinoma. Up to 70% of women suffer from non-cancerous breast diseases, and any of them can also increase the risk of malignant transformations.
Breast density. Women with mammographically denser breasts (with less fat but more glandular and fibrous tissue) are at a higher risk of developing breast cancer. Increased breast fibrosis can increase the risk of various subtypes of breast cancer by four to six times * *.
Injuries. Women who have previously received radiation in the chest area, for example associated with radiation therapy for another cancer, have a significantly higher risk of developing breast cancer. The increased general inflammatory level caused by chronic inflammatory diseases and other aggressive factors has a carcinogenic effect on epithelial cells, including breast cells.
Mechanical trauma to the breast tissue can also pose a risk of cancer. This may be due to various reasons, such as an inflammatory condition, blockage of the blood supply, and many others.
Implants. There is no conclusive evidence that breast implants alone increase the risk of cancer. However, women with cosmetic breast implants who develop breast cancer have more than a 25% increased risk of being diagnosed at a later stage compared to women without implants. This can be caused both by possible changes in the tissues caused by the operation and the implant itself, or by the implant masking the manifestations of early symptoms of breast cancer.
Hormones are molecules that are able to bind to their respective receptors on the cell surface, thereby activating them. As soon as the receptor is activated, it moves into the nucleus of its cell to certain sections of DNA. By attaching to its target genes on chromosomes, the activated receptor either blocks, or vice versa, starts the processes of creating certain proteins that control the behavior of the cell, including reproduction and death.
Breast cancer is sensitive to several sex and growth hormones (including estrogens, androgens, progesterone, prolactin, and insulin-like growth factors), and each of the breast cancer subtypes is characterized by both unique and specific hormonal influences *. Approximately 80% of all breast cancers show increased expression of progesterone and/or estrogen *.
Thus, all reproductive factors that are able to increase the duration and/or levels of exposure to hormones that stimulate the growth of breast cells increase the risk of breast cancer.
Oral contraceptives (OCs) may increase the risk of developing breast cancer *. Numerous studies give differing results. In one, the relative risk increased from 9% after one year of use to 38% after use over the last 10 years *. According to another, compared with women not taking OCs, women taking them have an increased risk of breast cancer – 2 times when taken for less than 6 years in a row, and 3 times when taken for more than 6 years *. Since stopping the pills, the risk has gradually decreased.
A meta-analysis of 34 case-control studies indicates that OC use was associated with an increased risk of breast cancer in premenopausal women. Overall, the risk increased by more than 19% *. Most of all (up to 52%), oral contraceptives increased the relative risk of breast cancer in those giving birth women who used them 4 or more years before the first full-term pregnancy.
Another study reported that the earlier a woman starts using OCs, and the longer she does so, the higher the risk. In women younger than 45 years, oral contraceptive use for 6 months or more was associated with a 30% increase in the relative risk of cancer. Those who started using OCs before the age of 18 and continued to use them for more than 10 years had a three-fold increased relative risk compared to women who did not use OCs. Those who used OCs within 5 years of being diagnosed with cancer also had a higher risk than those who did not take them *.
Of particular concern are reports that OC use for more than one year is associated with a 2.5-fold increase in the risk of the most dangerous subtype, TNBC * *.
Reproductive period. The increased risk may be due to the increased duration of estrogen exposure. The more menstrual cycles a woman has in her life, the higher her risk of developing breast cancer.
Women who start menstruating at an early age (before age 12) and/or start menopause at an older age (after age 55) have a higher risk of developing breast cancer. Each year of delayed onset of menarche or each subsequent birth reduces the risk of breast cancer by 5% or 10%, respectively *. Thus, the longer the period from menarche to menopause, the higher the risk of cancer.
High birth weight, accelerated development, and rapid height growth during puberty * are also risk factors. We have little ability to influence these events without side effects, but they can be alleviated to some extent through high physical activity, plant-based protein and fiber intake, and avoidance of alcohol.
Pregnancy, childbirth and lactation. The sex hormones associated with pregnancy increase the volume and density of the breasts, and make the tissues inside the breast less fat and more glandular. This increases the risk of developing benign breast changes.
On the other hand, the first pregnancy leads to the final differentiation of mammary duct cells *, and differentiated cells are 20 times less prone to division *. Thus, reducing the time gap between the appearance of the first menstruation and the birth of the first child reduces the risk of tumors. And since the final differentiation of breast cells occurs during the last trimester, the artificial termination of the first pregnancy, on the contrary, increases the risk.
Women who have not had children or who have a pregnancy at a later age (> 35 years) are 1.5 times more likely to develop breast cancer than those who have a pregnancy at an earlier age (< 20 years) *. In general, it is believed that pregnancy slightly increases the risk of breast cancer in the short term, but markedly reduces it in the long term *.
These observational studies are supported by experiments on rats. When injected with an equal amount of cancer cells, virgin female rats had an 18% to 100% risk of developing cancer (inversely related to age), while females that already had two cycles of birth and offspring had zero risk *.
Another benefit of pregnancy is that it reduces the lifetime number of menstrual cycles during which levels of carcinogenic estrogen (estradiol) rise. During pregnancy, the level of other estrogens increases, but they are less carcinogenic compared to estradiol.
Breastfeeding is associated with lower estradiol levels and higher prolactin levels up to 12 weeks postpartum *. In addition, breastfeeding causes an increase in the uptake/presence/transit of iodine into breast tissue. Due to this, increasing the lactation period to 1 year more may reduce the risk of developing breast cancer, and offset the adverse effects of the previous months of pregnancy. Indeed, a meta-analysis shows that exclusive breastfeeding among women who have given birth reduces the risk of breast cancer compared with women who have given birth and who do not exclusively breastfeed *.
It has been observed that breastfeeding is associated with a reduction in ER– tumor subtypes, while the number of full-term pregnancies (parity) is associated with a reduced risk of ER+ tumor subtypes *.
Chemical pathogens. Certain xenoestrogens, carcinogens, and endocrine disruptors, including those associated with the work environment, may be associated with breast cancer. For example, the use of diethylstilbestrol (a drug commonly prescribed to pregnant women to prevent miscarriage from 1940 to 1971) may slightly increase the risk of developing breast cancer. Women whose mothers took diethylstilbestrol during pregnancy may also have a slightly higher risk of breast cancer.
There are many toxins that exhibit carcinogenic effects, including heavy metals such as cadmium, nickel, cobalt. The aluminum salts found in antiperspirants are metalloestrogens and can also increase the risk of breast cancer *, especially if applied directly after shaving underarms *.
Increasing pollution of the planet with microplastics is of increasing concern. Harmful exposure to microplastics can occur through ingestion, inhalation, and skin contact with microplastics due to their presence in food, air, and water. The inability of the immune system to remove synthetic particles can lead to chronic inflammation and an increased risk of cancer.
The circadian rhythm regulates the daily cycle of processes occurring in the cells of various organs. Including, their proliferation and apoptosis, cell cycle, cell metabolism, as well as the survival of breast stem cells *.
Approximately 600 genes are under circadian control in the breast, and disruption of their expression can alter the biology of the breast and contribute to the development of cancer. The amplitude of oscillations of the circadian clock is controlled by the biomechanical rigidity of the stromal tissue. A special study revealed a disruption in the circadian rhythm in breast cancer cells compared to normal cells from the same patient. This correlates with increased tissue stiffness around the tumor area and suggests a detrimental effect of circadian disturbances on the development and progression of breast cancer *.
Circadian disruptions caused by late wake ups and shifting night shifts, as well as other hormonal disturbances, including excess insulin (due to excess sugar) or cortisol (due to stress), also lead to hormonal imbalances, indirectly affecting sex hormones, in including a drop in progesterone and a rise in estrogen. Which, in turn, promotes cell proliferation and an increased risk of breast cancer.
Physical activity. High physical activity reduces the level of insulin and insulin-like growth factor. Regular physical activity for 4-7 hours a week can reduce the risk of breast cancer. Conversely, according to meta-analyses, sedentary work is associated with a 15% increase in the relative risk of breast cancer *. For every hour of sedentary activity per day, there is an estimated 1% increase in breast cancer risk *.
Bad habits. Alcohol consumption depletes the body of vitamin B12 and increases the risk of breast cancer linearly; and this happens, it seems, without any safe threshold level.
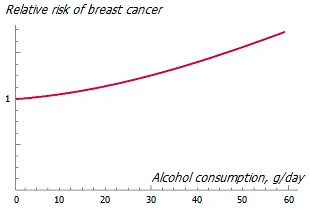
For this reason, the International Agency for Research on Cancer has classified ethyl alcohol as a carcinogen *. Drinking 35-44 g of alcohol per day can increase the risk of breast cancer by 32% compared to non-drinking women, with a relative risk increasing by 7.1% for every additional 10 g of alcohol per day * *.
Alcohol consumption increases the risk of ER-positive breast cancer in women *, especially in postmenopausal women * *. A positive relationship has been found between alcohol consumption and endogenous estrogen levels and mammography density in premenopausal women *. In addition, alcohol consumption after a breast cancer diagnosis is associated with both an increased risk of breast cancer recurrence after treatment and an increased risk of patient death *.
Smoking can significantly increase the relative risk of lung cancer in smokers compared to non-smokers; but compared to lung cancer, the relative risk of breast cancer in women who smoke is much lower. However, smoking significantly increases the overall inflammatory level, which indirectly contributes to the development of cancer and other degenerative diseases, as well as aging.
It is worth recognizing, of course, that relative risk only compares the risk between two different groups. When the absolute risk is small, in general terms, even a large relative risk may actually be negligible. For example, in terms of relative risk, smokers are seven times more likely to die from lung cancer than non-smokers. And in terms of absolute risk, smokers have a 3% chance of dying from lung cancer compared to a 0.4% chance for non-smokers. Compare for yourself two estimates of the same fact: «by 7 times» and «by 2.6%».
However, this does not at all justify addictions, because the resulting carcinogenic effect of various factors can multiply and, in the end, turn out to be a turning point.
Other risk factors and their combinations. Glucose intolerance, hypertension, dyslipidemia, and BMI ≥ 27.7 kg/m2 are found in a quarter of patients with breast cancer. Diabetes, glucose intolerance, and dyslipidaemia (increased plasma levels of cholesterol and/or triglycerides) are associated with a higher risk of metastatic cancer recurrence. The presence of three or more metabolic comorbidities is also strongly associated with the risk of recurrence of metastatic disease, especially in luminal B-subtype cancer and in postmenopausal women * *.
Nutrition requires special consideration, since it is the diet that is the most influential and most easily changeable environmental factor. The presence of various types of carcinogens in food products can be caused by various reasons: their natural presence in raw materials; contamination during cultivation or storage; intentional addition during preliminary preparation and storage; finally, their natural formation in the process of culinary processing.
Excessively present in the diet of a modern person, sugar causes the release of excess insulin into the blood, and insulin is a powerful factor in cell growth. Foods high in calories, low in fiber, and rich in processed meats, especially saturated fat, dramatically increase the risk of breast cancer *.
Sensitivity to milk protein or gluten found in wheat can affect up to 15-17% of the general population, and there are many other foods that can cause individual sensitivity that can cause an inflammatory response.
Different risk factors have different strength of significance on the risk of breast cancer.
Factors that increase the relative risk (RR) of breast cancer in women * |
|
RR |
Factors |
>4,0 |
Age (>65 years versus <65 years) Biopsy-proven atypical hyperplasia Certain inherited genetic mutations for breast cancer (BRCA1 and/or BRCA2) Non-invasive ductal carcinoma Non-invasive lobular carcinoma Mammographic breast density (most dense versus least dense) Personal history of early-onset breast cancer (<40 years) Two or more first-degree relatives with breast cancer diagnosed at an early age |
2,1-4,0 |
High levels of endogenous estrogen or testosterone (postmenopausal) High dose chest radiation One first-degree relative with breast cancer |
1,1-2,0 |
Alcohol consumption Exposure to diethylstilbestrol Early onset of menarche (<12 years) Growth (high versus low) High socioeconomic status Late age at first term pregnancy (>30 years) Late menopause (>55 years) Lack of breastfeeding No term pregnancies Obesity (postmenopausal) Breast hypertrophy without atypia (usual ductal hyperplasia and fibroadenoma) Recent and long-term use of menopausal hormone therapy containing estrogen and progestin |
Each woman, taking into account her individual characteristics, can calculate the relative 5-year * or lifetime * risk of cancer using the appropriate online resources.
Each of the risk factors, to one degree or another, contributes to the total risk of disease *. The more we collect minuses in the karma of our illness, the higher the likelihood that we will win this damned lottery.
Each of these, or the sum of any of them, may be the main cause of cancer in already diagnosed women. It is not known exactly which of them. There are factors that are beyond our control (such as gender or heredity), and there are factors that we can change (such as nutrition or giving up bad habits). The more of them to delete from your life, the higher the likelihood of not getting cancer. And the higher the chance to get rid of it. The cancerous process, despite its formidability, is not unstoppable and irreversible * * *, which gives us healthy optimism.