Health Strategy.
Vitality is fullness of health and inner strength. The higher the vitality, the healthier a person looks and feels, the more vital energy he has. Strengthening the general condition, increasing vitality reduces the chances of morbidity and increases the success of treatment.
The following points are suggested to achieve this goal:
• Normalization of body weight
• Post
• Normalization of blood pressure
• Detoxification and organ support
Most of them are in line with the recommendations of the World Cancer Research Foundation and the American Institute for Cancer Research (WCRF/AICR) for cancer prevention *:
1. Normalization of body weight. Maintaining a body weight appropriate for age 21.
2. Moderate physical activity. Physical activity equivalent to brisk walking for at least 30 minutes daily.
3. Low-calorie food. High-calorie foods include foods with an energy content of 225 kcal per 100 g or more.
4. Plant food. Daily at least five servings (at least 400 g) of various non-starchy vegetables, fruits (at least 400 g), grains and legumes – with each meal (at least 25 g).
5. Restriction of products of animal origin. Less than 500 grams per week of red meat, and less than 25 grams per week of processed meats.
6. Minimize alcoholic beverages. No more than a glass of dry red wine per day.
7. Storage, processing and preparation of food. Avoid food cooked on an open fire; limit the consumption of table salt (below 5 g/day); Avoid exposure to mold toxins from moldy cereals (cereals) or legumes (peanuts) whenever possible, and avoid prescription drugs.
8. Biologically active additives. Dietary supplements for cancer prevention are not recommended.
Following these recommendations can significantly reduce the risk of breast cancer, as well as reduce mortality in patients already diagnosed * *, especially postmenopausal women *. Compliance with each additional recommendation was associated with an average 11% reduction in breast cancer risk, but among them, the recommendations to increase physical activity and reduce animal food intake were the most significant in reducing risk: 16% and 21%, respectively. Women who followed 6-7 recommendations had a 51% lower risk of breast disease compared to women who followed no more than 2 recommendations *. It is estimated that at least half of breast cancer cases can be prevented with simple dietary and lifestyle changes *.
According to another similar study, following each of these recommendations reduces the relative risk of general cancer by 5% *. Here, women who followed 4-6 recommendations had a 16% lower risk of breast cancer than women who followed less than 3 recommendations. Despite the difference in statistical data, the trend of both studies is the same.
Following the WCRF/AICR guidelines not only reduces the risk of cancer, but also reduces all-cause mortality among older women who have had cancer *. Women who followed the highest number of recommendations (6-8 items) versus those who completed the fewest (up to 4 items) had a 33% lower all-cause mortality rate over 5 years and a 39% lower cancer mortality rate mammary gland. Adherence to the recommendation for moderate physical activity was the strongest factor associated with a lower risk of mortality.
Along the way, following these recommendations significantly reduces the risk of death, cardiovascular and respiratory disease, and increases longevity *. A combination of at least four healthy lifestyle factors (weight loss, alcohol restriction, smoking cessation, healthy diet, and physical activity) is associated with a 66% reduction in all-cause mortality *.
The combination of a plant-based diet and moderate exercise almost doubled the survival time of breast cancer patients compared to either method alone. The greatest successes in reducing mortality have been achieved in women with obesity, as well as those with ER+ and PR+ tumors *. Overall, the combination of a vegan diet, exercise, weight management, hormone replacement therapy, and elimination of addictions can add up to 10 years of life expectancy in women compared to the average life expectancy in the local population *.
Physical activity has the strongest influence of any lifestyle factor affecting both the risk of breast cancer * and the risk of recurrence *. The result of muscle exercise is a decrease in glucose levels, sex hormones, inflammation and insulin resistance. In addition, regular moderate-intensity exercise increases the efficiency of immune T-cells * and natural killer cells * *.
An eight-year prospective study found that people who performed 15 minutes of daily exercise had a 14% reduction in the risk of all-cause mortality compared with inactive people. In addition, their life expectancy increased by 3 years. Every additional 15 minutes of exercise above that reduced all-cause mortality by an additional 4% *. With daily 90-minute sessions, the maximum effect was achieved.
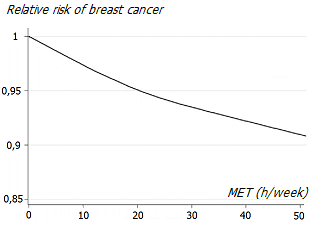
Low versus high levels of physical activity increase the incidence of breast cancer by 11.6% *. Conversely, moderate physical activity after diagnosis is associated with a 34% reduction in the risk of cancer death, with a 41% reduction in the risk of overall mortality and a 24% reduction in the risk of recurrence compared to controls *.
An activity corresponding to walking at an average pace of 3-5 hours per week, compared with less exercise, reduces the absolute 10-year risk of death for women with breast cancer by 6%. The relative risk of adverse outcomes (death and recurrence of breast cancer) was 26-40% lower compared to women with the highest and lowest activity category. This association was especially pronounced in women with hormone-sensitive tumors *.
A meta-analysis of 22 observational studies concluded that breast cancer mortality decreased by more than 40% among women who participated in remedial physical activity after diagnosis of the disease, compared with women who did not participate in reactivation. However, the effect was more pronounced in women who met the recommended levels of physical activity, in postmenopausal women and in obese women *.
A sedentary lifestyle is detrimental to estrogen balance and promotes estrogen dominance. Whereas weight loss promotes favorable changes in the earliest tumor biomarkers such as estrogens, inflammatory markers and sex hormone binding globulin. Regular strength training can increase testosterone levels, reduce androgen and estrogen imbalances, and reduce the side effects of hormone therapy such as weight gain, loss of muscle and bone mass.
Muscular load of medium intensity:
- improves mood;
- enhances breathing and blood oxygenation;
- reduces the concentration of glucose in the blood;
- significantly reduces inflammation by reducing the level of arachidonic acid;
- reduces the level of estrogen;
- normalizes testosterone levels;
- improves lymph circulation and sweating, reducing the overall toxicity of the body;
- helps shed body fat that stores toxins and produces estrogen and pro-inflammatory molecules.
The recommendations approved by the American Cancer Society * suggest at least 30 minutes of moderate-intensity physical activity at least five days a week, or 75 minutes a week of more intense exercise, including exercises for major muscle groups. The duration of each activity should be at least 10 minutes. Longer (but not more strenuous) exercise may bring more benefits * *. Optimal results are achieved with a combination of both aerobic and resistance exercise *.
Unlike many therapeutic manipulations, physical activity does not cause any negative side effects. The problem, however, may be that physical activity causes an increase in appetite, and for obese people, they require significant effort. Both reduce the desire to exercise, and the initial beneficial impulse often fades away. In addition, patients usually feel unwell and tired, which does not stimulate additional physical activity. Thus, in addition to volitional efforts for training, it is required to choose such a training that would not be a burden.
Lots of low-intensity movement throughout the day is recommended, such as walking, jogging, gentle cycling, light dancing, toning sports (eg table tennis), etc. And also periodic intensive exercises for resistance and tension, swimming. Jumping on a trampoline is excellent for enhancing circulation and cleansing the lymph.
Despite the usefulness of an active lifestyle, an elementary calculation shows that in order to maintain energy balance, it is much easier to avoid calories than to burn them through physical activity. A whole hour of moderate-intensity exercise or ballroom dancing will take only about 300 kcal, which is easy to get by just spreading butter on one or two sandwiches. It is impossible not to store energy in the form of fat if you consume more than you expend. This is a simple law of conservation of energy.
Normalization of body weight. Obesity exacerbates the severity of almost all diseases and increases the risk of all-cause mortality. In a meta-analysis of data from 139 studies, weight loss was associated with an 18% relative reduction in breast cancer risk *. Another meta-analysis of 79 published studies found that, compared with women of normal weight, patients who were obese or overweight at diagnosis had lower survival and higher mortality from breast cancer *. Obesity leads to a reduction in life expectancy by an average of 8-10 years compared to people with normal weight, and every 15 extra pounds increases the risk of premature death from all causes by about 30% *.
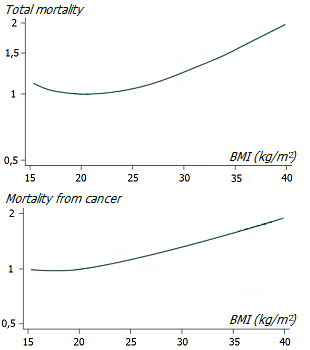
A high body mass index, at least in postmenopausal women, increases the risk of breast cancer more than inactivity, smoking, and even more than lifetime alcohol consumption *. Overweight or obese postmenopausal women have a 2.5 times higher risk of developing breast cancer compared to normal weight women * * *. In premenopausal women, being overweight increases the risk not so dramatically, but, nevertheless, quite strongly – up to 30%. But in postmenopausal women, even with a normal body mass index, every 5 kg of total body fat increases the risk of invasive ER+ breast cancer by 35% *.
Body fat, especially in the abdominal cavity, may contribute to increased risk and worse prognosis in several ways: increased circulating insulin-like growth factor, increased levels of circulating sex hormones, C-reactive protein and pro-inflammatory cytokines * *. In turn, inflammation promotes weight gain at the expense of fat, which creates a vicious cycle *. Many pathogens are fat-soluble, and fat serves as both a vehicle and a storage site for them. In addition, fat cells in breast tissue express aromatase, which increases local estrogen production, increasing the risk of hormone-sensitive cancer.
Loss of total body fat through diet and exercise is associated with beneficial changes in free estradiol, free testosterone, leptin, and sex hormone-binding globulin (SHBG) – different types of biomarkers known to be associated with breast cancer risk *. At the same time, markers of systemic inflammation are reduced *.
Most breast cancer patients gain weight (usually 2.5-5 kg) both during and after therapy, much of which is never lost. And many have excess fat already before treatment. The main causes of weight gain are called: endocrine disorders; excess calories in food; insufficient energy costs; systemic inflammation; stress; poor quality sleep; reduction of stressful changes in ambient temperature; sharp refusal of smoking; use of drugs that cause weight gain; belonging to a social, ethnic and age group prone to obesity; genetic and epigenetic risk factors that are inherited; late pregnancy of the mother.
The recommendation to maintain body weight refers to cases when it is within the normal range. In the case of already existing obesity, a decrease in body mass index may require a set of active measures, which is discussed in the additional chapter – «Weight Loss Program» †.
Diet modification includes changing the structure of the diet and changing the mode of eating.
The change in the structure of the diet consists in reducing the total caloric intake, increasing the proportion of hidden water and fiber in the food taken, while minimizing the proportion of fats (especially animals), as well as reducing the ratio of solid food to liquid in favor of the latter. All this has already been discussed earlier, in the section «Diet Therapy» †.
Observational studies show that sugar and meat consumption are the two most significant and roughly equal contributors to the prevalence of obesity *. An increase in animal or poultry meat consumption of 250 g/day (e.g. one steak) over 5 years results in a weight gain of 2 kg * and this relationship is independent of total calories consumed and physical activity value *. Just avoiding animal food and minimizing fat intake can lose about 6 kg of excess weight in 14 weeks, at least in postmenopausal women *. This result is much higher than the result of any of the weight loss products offered by the helpful market.
Excess consumption of fats and simple carbohydrates can also negatively affect the metabolic and hormonal processes (for example, by increasing estrogen levels) that affect the development of breast cancer metastases * *. Excess caloric intake has been shown in rodent studies to accelerate the growth of breast tumors even in the absence of estrogen *. In initially lean people, an increase in calorie intake in the form of fat leads to an increase in overweight much more easily than an increase in calorie intake in the form of proteins or carbohydrates *.
Refined foods, by creating an excess of calories while deficient in many important nutrients, contribute to weight gain. The emerging deficiency of essential elements, the body tries to get by increasing the amount of food consumed. In addition, excess calories increase insulin levels, giving an internal signal for the period of fruit ripening and subsequent winter hunger, which also stimulates the storage of energy in fat.
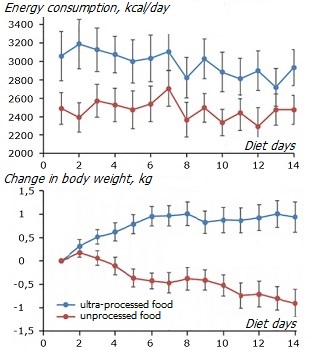
One study shows that with 2 weeks of unrestricted feeding, energy intake increases with a diet high in ultra-processed foods (+508 kcal/day), as well as with increased intake of carbohydrates (+280 kcal/day) and fat (+230 kcal/day), but not protein (-2 kcal/day) *. While the study participants gained 0.9 kg on the ultra-processed food diet, they lost 0.9 kg on the unprocessed food diet.
Limiting the consumption of ultra-processed foods may be an effective strategy for not only treating obesity but also preventing cancer. For every additional 10% of calories from highly processed foods, there is a 10% increase in cancer risk *.
Fats are a greater source of calories than proteins and carbohydrates of the same weight. For this reason, limiting fat intake as much as possible will play a greater role in limiting dietary calories. The composition of dietary fat also matters. For example, a diet enriched with olive oil may lead to greater weight loss than a diet low in fat *.
Dieting, as it is widely understood, means the temporary restriction of certain foods. However, even in cases where, at the cost of effort and deprivation, it leads to some weight loss, upon returning to normal nutrition, the weight almost always bounces back. Two-thirds rebound within one year, and nearly all within five years *.
None of the trendy diets regularly featured in popular women's magazines work. And they can't work. If this were not so, then every month a new and new diet would not be published, causing not weight loss, but only discomfort and disappointment. And many of them bring only harm. They bring unconditional benefit only to the owners of magazines selling empty hopes.
«Willpower» also does not work and cannot work. Hunger is the strongest of all human instincts; it is stronger than the instincts of reproduction and self-preservation. In addition, severe food restrictions through a complex psycho-hormonal connection are perceived by the brain as a loss of food availability, which psychologically stimulates an even greater increase in calorie intake. Sharp short-term restrictions on caloric content of food lead to the fact that after their end, the body, instead of reducing fat reserves of fat, stimulates the accumulation of fat, waiting for new periods of starvation to come soon.
For this reason, many calorie-restrictive diets as a means of losing weight are not only ineffective, but are also a direct cause of subsequent weight gain *. Even when they successfully lead to initial weight loss, one-third to two-thirds of participants gain more weight than they lost *. Only 20% of those who have lost 10% of their body weight due to the diet will be able to maintain this achievement within a year after stopping this diet *. This implies the importance of not only losing weight, but also the importance of maintaining this loss.
While dietary calorie excess is a major part of the weight problem, calorie reduction is an overly simplistic way to solve it. In fact, this is an important, but still insufficient condition. It is believed that there is a so-called "set point" of calorie intake, which the body considers necessary to obtain in order to maintain existing weight. And any reduction in energy consumption will include compensatory mechanisms to achieve it. So, the deviation of the level of hormones responsible for the feeling of hunger is observed even a year after the end of the restrictive diet * *.
Therefore, temporary calorie restriction is unlikely to help you lose weight permanently. Really stable weight normalization can be achieved if low-calorie nutrition becomes not a temporary measure, but a stable long-term norm that can move down the «set point». A low-energy diet not only reduces energy intake, but also helps to maintain weight loss. Unfortunately, without reducing hunger, it is very difficult to stick to a low-calorie diet.
Because of the existence of a «set point», it is advised to reduce the caloric content of food consumed gradually but steadily. At the same time, the rate of weight loss should not exceed 1'200 grams per week. If the weight, despite all efforts, does not fall, then either the intake of calories still exceeds their consumption, or there are serious hormonal problems, primarily with the thyroid gland.
Dietary changes that promote weight loss should create a feeling of abundance and satiety while providing adequate nutrition and limiting fat and calorie intake.
The transition to a new, unusual diet takes several weeks and, as a rule, is accompanied by psychological discomfort. It takes time for the body to rebuild its metabolism from the usual food to a new one. Worst of all is the restriction of animal protein and sugar. Meat and dairy products provide the body with «fast» amino acids that do not require complex synthesis, in the same way that sugar provides «fast» glucose. Sugar is just as addictive as soft drugs; and the rejection of sugar is accompanied by a state somewhat similar to the «breaking» of a drug addict.
Replacing sugar with sweeteners is a bad idea. Sweeteners disrupt the dopamine system *, contributing to depression; reduce sensitivity to sugar *, stimulating an increase in calorie intake *; increase the risk of diabetes * and are extremely detrimental to the intestinal microflora * even at doses that the FDA considers acceptable. In severe cases, stevia, licorice root and chicory root, added to drinks instead of sugar, will help to cope with temporary difficulties. Reducing stress also reduces sugar cravings.
However, food is not just a source of calories. It's a pleasure, it's an opportunity to communicate, and to a large extent it's a ritual. It is important for a person that with a minimum of calories, food is satisfying and tasty. That it causes satisfaction, not discomfort. Therefore, in addition to simply reducing calories, it is worth paying attention to other aspects of nutrition.
The change in the mode of eating. It is important not only the total caloric content of the food taken, but also the diet, even with the same diet. Early research gave rise to well-established medical In addition to frequency, the distribution of daily energy intake, calorie restriction and the length of the break between meals (especially at night) and the timing of meals are important. The physiological basis for these interrelated factors is the synchronism of food intake with natural circadian rhythms and the body's need for energy and nutrients. Changes in meal frequency and timing can affect energy and macronutrient absorption and lead to metabolic syndrome *.
• Eating regularity, consuming most of the calories in the morning, reducing the frequency of meals (up to 2-3 times a day), 5-6 hour break between breakfast and lunch, long night break (12-18 hours), compliance of the consumed products with the current season and regular periods of short-term fasting can provide positive changes such as reduced inflammation, improved circadian rhythm, increased autophagy and cellular stress tolerance, and a healthier gut microflora *.
An increase in the duration of the nighttime fasting reduces the ratio of the time of active metabolism to the time of cleansing from its end products. Limiting food intake later in the day reduces total daily energy intake *. Increasing the duration of overnight fasting to more than 11 hours, in one study, reduced the weight of patients in the control group compared to the experimental group by only 1.3% *.
Every 3 hours of prolonged fasting at night is associated with a 19% reduction in the likelihood of an increase in glycated hemoglobin (HbA1c) *. In addition, increasing the time between dinner and breakfast to 14-15 hours significantly improves glucose tolerance in diabetics even without changing their usual diet * *, reduces the level of such an inflammatory marker as CRP * by 8%, and allows to reduce within 16 weeks body weight by an average of 3 kg, which remains unchanged over the next 36 weeks *.
Finally, in the group of patients with early stage breast cancer, overnight fasting of more than 13 hours was associated with a 36% reduction in the risk of breast cancer recurrence compared to patients with an overnight fast of less than 13 hours *.
• Frequency of eating is controversial. Some research suggests that eating more frequently, reducing energy intake in the evening, and fasting for longer nightly intervals may reduce systemic inflammation and subsequently reduce the risk of breast cancer *. This is easily explained by the fact that frequent consumption of low-glycemic foods allows you to keep blood glucose levels at a more or less stable level, avoiding its sharp spikes and the associated increase in the level of free radicals and inflammatory molecules.
Other studies show that high meal frequency (6 or more meals per day) versus low meal frequency (1-2 meals per day) may be associated with a significant increase in disease risk *. There was no explanation for this result.
• The distribution of caloric content of food by time of day corresponds to traditional recommendations. The largest amount of calories should be in breakfast, i.e. before the start of intensive calorie expenditure during the day *. This recommendation does not distinguish between different chronotypes of people («larks» and «owls») *. Shifting the timing of calorie intake closer to the start of the rise in melatonin levels significantly increases body fat percentage and body mass index *.
Animal studies show that eating fatty foods during an inactive period, especially in the evening, leads to weight gain and metabolic syndrome. At the same time, skipping dinner contributes to an increase in total daily food intake and a set of body fat mass *. At the same amount of daily food, weight gain and insulin levels are suppressed in the 2-meal group (higher-calorie breakfast + lower-calorie dinner) compared to the 1-meal group (breakfast only) *.
Similar results have been observed in humans. Morning food intake is especially satiating and can reduce the total amount consumed throughout the day *. In the weight loss groups, shifting lunch later than 3:00 pm caused worse weight loss compared to shifting lunch earlier than 3:00 pm *. Those who consume ≥ 33% of their daily calories in the morning are half as likely to be overweight as those who consume ≥ 33% of their daily calories in the evening *. The higher-calorie breakfast and lower-calorie dinner group had better scores for many metabolic markers, body weight, fasting blood glucose and insulin levels, and satiety than the lower-calorie breakfast and higher-calorie dinner group *.
Those who eat breakfast regularly are less likely to gain weight than those who constantly skip breakfast. And those who have the most calories at lunch or dinner have a greater risk of increasing their body mass index *. In both lean and obese people, a daily breakfast, compared to abstaining from it, provides increased physical activity and endurance, increases insulin sensitivity, providing more stable daytime and evening glycemia, and avoids high calorie intake at night * *.
A seven-year study of the diet of 50'660 people over 30 showed that, compared with 3 meals a day, one or two meals a day can reduce body mass index, while more than 3 meals a day (or snacking) increases it. Those who don't skip breakfast also experience weight loss compared to those who skip it. Those who took in the most of their daily calories at breakfast experienced the greatest weight loss compared to those who shifted the most calories to dinner *. Skipping breakfast and eating late in the evening have been associated with an increased risk of obesity in many studies * * *.
In addition, postponing meals significantly increases serum triglyceride and LDL levels *. Data from 51'529 healthy men over 16 years of follow-up concluded that eating breakfast was associated with a significantly lower risk of developing coronary heart disease. Men who skip breakfast have a 27% higher risk of developing coronary heart disease than men who eat breakfast regularly. And eating late at night is associated with a 55% increased risk compared to eating earlier *. Unfortunately, in industrialized countries, the proportion of calories in food increases in the evening, and dinner accounts for the majority (up to 40%) of all daily calories *.
Based on the foregoing, it is proposed to have breakfast mainly with fats (nuts) and «slow» carbohydrates (grains, legumes, chia, flax, redhead), dine with more high-calorie vegetables (potatoes, beets, cabbage), and dine mainly with less calorie vegetables, as well as other low-calorie meals (smoothies, greens, raw and cooked vegetables, berries, yogurt) and protein (fish, vegetable curd).
Despite prolonged night fasting, hunger and appetite are usually greater in the evening than in the morning, regardless of daily food intake and physical activity *. However, by shifting to dinner an easily digestible protein that quickly induces a feeling of satiety *, the volume and calorie content of the evening meal can be reduced. In addition, you can reach a feeling of fullness faster, and thereby reduce the calorie content of the food you eat, if you start your meal with bulky, high-fiber dishes, such as vegetable salads.
The American Dietetic Association is also of the opinion that "consuming more energy during the day may be preferable to evening consumption" *. Many amateur (Cronometer, Dr. Greger's Daily Dozen, MyNetDiary,MyFitnessPal, MyPlate Calorie Tracker) and more professional (Diet Pro, Nutrium, A la calc, Genesis R&D Food Labeling) software applications make it easy to track calories and nutrition structure, and also help in compiling a daily or weekly menu.
A low-calorie diet, a high level of physical activity, constant weight control, regular breakfast and a stable diet help to fix the weight reduced as a result of previous manipulations; and adherence to such a regimen for 2-5 years further increases the chance of long-term success *.
Fasting is considered the most effective natural manipulation that can prolong life and health, delaying the development of not only cancer, but also other degenerative diseases. Throughout the animal kingdom, intermittent fasting occurs naturally depending on the availability of food at the time. This variable calorie regime seems to be consistent with the diet of our hunter-gatherer ancestors. Based on this, it can be assumed that our bodies are evolutionarily tuned for intermittent fasting, or intermittent feeding, and not for a stable supply of food.
Short-term fasting (up to 3 days) does not cause ketosis, while longer fasting is accompanied by ketosis. After this period, glucose stores are depleted, and glycogen stores are no longer sufficient. And so the body switches to alternative energy sources such as fats.
Therapeutic fasting differs from therapeutic calorie restriction by temporarily cutting out food altogether rather than permanently reducing daily calorie intake. At the same time, there are a variety of forms of fasting, differing in duration and severity. The most effective will probably be the cyclical alternation of normal food with fasting *: fasting for 24 hours twice a week or 48 hours once a week. The transition to a new diet is accompanied by an uncomfortable transition period of 3-6 weeks, during which the brain and body adjust, losing the habit of daily eating * *.
While chronic calorie restriction can cause unacceptable weight loss in cancer patients and is therefore considered inappropriate *, short periods of fasting have been shown in preclinical studies to be beneficial in cancer * * *. The fact is that during short-term fasting, the susceptibility to chemotherapy of healthy somatic and cancer cells turns out to be different * *; this phenomenon is called differential stress resistance *.
Under conditions of nutrient restriction, cells are forced to save energy, and spend it not on growth and division, but on ensuring their survival. Calorie restriction may provide protection against invasive breast cancer in women in many ways *, including by reducing inflammation *.
Intermittent fasting causes a decrease in blood glucose, insulin, and insulin-like growth factor I (IGF-I) *, and also activates autophagy * * and promotes stem cell-based immune system regeneration upon refeeding *. Together, this makes many types of cancer cells more sensitive to chemotherapy * *.
The practice of intermittent fasting can have a powerful effect on cleansing and detoxifying cells and the entire body. Even short-term fasting on water (1-2 days in a row within a week) stimulates the process of autophagy (self-eating), during which cells begin to cleanse themselves, metabolizing misfolded proteins and other pathogenic accumulations that contribute to inflammation and cancer. However, fasting for more than 3 days may be counterproductive and increase tumor malignancy *.
The effectiveness of intermittent fasting was comparable to a permanent calorie restriction regimen. Two cycles of intermittent short-term fasting (2 days per week) halved the growth of mouse triple-negative mammary tumors in mice, and the combination of fasting with chemotherapy reduced its growth by 5 times compared with control *. Insignificant weight loss of animals during fasting days was quickly compensated during the period of normal feeding.
Intermittent fasting shows 3-8% weight loss after 3-24 weeks, while calorie restriction shows 4-14% weight loss after 6-24 weeks. Both of these weight loss strategies result in comparable reductions in abdominal fat mass, insulin resistance, and significant reductions in fasting glycogen concentrations *. Eating once a day for 8 weeks results in 4.1% more weight loss than eating three times a day on a low-calorie diet * *.
Circadian rhythm. Human is a diurnal species of animals, and the intensity of various biological processes in the body is subject to cyclic fluctuations associated with the change of day and night. They are called circadian, and they are a kind of internal clock task manager of the body *. The circadian function allows for anticipation and planning of daily routine processes, which greatly improves the efficiency of resource and energy use.
The internal biological clock of the whole organism is regulated by the hypothalamus, obeying the day:night cycle *. The central factor in the regulation of diurnal fluctuations in cell activity is sunlight (mainly the blue part of the spectrum), which, through the photoreceptors of the eyes, signals the daylight hours.
Tissues and organs whose function is regulated depending on the time of day (especially the intestines, liver, endocrine organs, adipose tissue, skeletal muscles) contain genes for peripheral timers. Peripheral timers work autonomously, but they can be slowed down/speeded up or set/reset by external signals, allowing cells to adapt to changing environmental conditions. The main dispatcher that synchronizes the work of peripheral timers is the central timer located in the hypothalamus, but its leading role can be weakened by many factors.
The circadian clock regulates over 40% of protein-coding genes * and imposes rhythms of the cell cycle and proliferation, metabolism, inflammation and DNA damage response *, including in breast cells *. They make all body systems work more coherently and efficiently.
Rhythmic gene expression has been found in virtually all tissues and organs of the body. Peripheral timer genes control appetite, bowel activity, nutrient absorption, metabolism, immune cell behavior, hormonal regulation, and bodily condition *. However, metabolism and circadian rhythms are connected not only by direct but also by feedback. Peripheral timers can be affected by a variety of external factors, including the fact of eating, rapid time zone changes, lengthening of the photoperiod, heat, physical activity *, and even the state of the intestinal microflora *.
Failure to follow the natural sequence of daily cycles (light:dark, activity:rest, wakefulness:sleep, nutrition:fasting) can disrupt the central and peripheral regulation of metabolic processes and the interaction of organs and systems, contributing to obesity and causing immune and hormonal disorders *. Daily fluctuations in body temperature, blood pressure, synthesis of hormones and enzymes can also be disturbed to some extent. For example, the amplitude of daily fluctuations in cortisol concentration may decrease, remaining at a fairly high level. And the nighttime amplitude of melatonin may, on the contrary, decrease.
Shift work, disrupting the circadian rhythm, promotes weight gain and other metabolic disorders *. In addition, dysregulation of the circadian rhythms of sleep and wakefulness is associated with an increased risk of breast cancer * * *. Based on this, the World Health Organization's International Agency for Research on Cancer (IARC) has designated shift work that disrupts circadian function as a probable class 2A carcinogen * *. Not only night shifts and entertainment are unacceptable, but also other night wakefulness.
The link between circadian rhythms and cancer is very telling. It has been reported that people who are completely blind (those with no photoreceptors working at all) have half the risk of cancer *. This is especially true of such hormone-sensitive types as breast cancer * and prostate *. The evening chronotype («owls») is associated with a 20% increased risk of breast cancer compared to the morning chronotype («larks») *. In women with breast cancer, a shift between preferred and actual sleep times is associated with accelerated disease progression *. Disruption of the circadian rhythm also worsens the prognosis in patients with breast cancer.
There is strong evidence that patients with intense and stable circadian rhythms live longer than patients with disturbed rhythms. Breast cancer patients with abnormally low diurnal fluctuations in cortisol have an increased risk of premature death *. On the other hand, nightly increases in melatonin levels as adjuvant therapy significantly improve tumor remission and 1-year survival rates *. In addition, a weak circadian rhythm increases the risk of neutropenia during chemotherapy in breast cancer patients *.
Recovery of circadian function includes waking up earlier (at sunrise) and going to bed early (a little after sunset); bright morning lighting (blue tint) and dim evening (red tint); sufficient solar exposure in the morning; reduction in caloric content and volume of food; shifting calorie intake and physical activity to the first half of the day; night period of low temperature, darkness, rest and fasting *.
Women with breast cancer who received 30 minutes of bright white light every morning improved their rhythmic activity and amplitude * and improved their quality of life during chemotherapy *.
• Melatonin is one of the most influential hormones of the circadian rhythm, and exogenous melatonin supplementation (3-15 mg strictly at bedtime) can largely compensate for its losses due to circadian disturbances. Melatonin is perhaps the only drug currently used to normalize the circadian rhythm.
• Dehydroepiandrosterone (DHEA), the so-called longevity hormone. Supplementation of DHEA (but not its sulfate) in the midday diet shortened the free circadian period in mice, which, given the reduced time of day, hastened their re-entry into the diurnal light:dark cycle *. The dosage used here was an order of magnitude higher than that recommended for humans as an anti-aging agent (50 mg/day in the morning) *.
• Caffeine * and theophylline * speed up the circadian rhythm, so for pre-menopausal women moderate consumption of coffee (2-4 servings) * *, cocoa or chocolate (10 g) * in the morning is quite acceptable, unlike their evening consumption. However, for postmenopausal women and BRCA1 mutation carriers, coffee consumption is not recommended *.
• Nobiletin and tangeretin, citrus peel flavonoids, have been shown to improve cell cycling in mice * at an oral dose equivalent to 18 mg/kg in humans. Unfortunately, nobiletin has very low water solubility and bioavailability *. And tangeretin can reduce the effectiveness of tamoxifen and the activity of natural killer cells *.
• Resveratrol, green tea polyphenols, and proanthocyanidins appear to improve circadian rhythm *, but the evidence base for their benefit is very weak.
• High salt content in food has a negative effect, lengthening the circadian rhythm and increasing the consumption of glucose by cells *.
In general, the use of bioactive substances to control the circadian rhythm is poorly understood, but the important role of food elements in this is clearly visible.
Mutations in the circadian clock genes have been found in tumor tissue of various organs, including the mammary gland *. Research suggests that the growth rate of breast cancer follows the rhythm set by the circadian clock *. However, extensive studies of the dependence of the mitotic activity of cells of various subtypes of human breast cancer have not yet been carried out.
Since the rate of division of cancerous and normal cells of the same tissue can peak at different times of the day, this can be used to enhance the effect of therapeutic agents (so-called chronotherapy). It has been reported that cisplatin in colon cancer is better tolerated (and appears to be more effective) between 16:00-20:00 *, and doxorubicin in ovarian cancer is better tolerated around 06:00 *.
Animal laboratory studies show that tolerability of ~ 30 anticancer drugs can vary by up to 50% depending on circadian rhythms. Clinical trials have confirmed the possibility of prescribing higher doses of chemotherapy with improved clinical outcomes while respecting chronobiological principles * * * *. However, the clinical application of chronotherapy is still a long way off.
Healthy spirit. The diagnosis and treatment of cancer, as well as the changes in personal relationships and the reassessment of values associated with them, are a serious psychological stress for the patient and his loved ones. Unmanaged chronic stress negatively affects almost all internal biosystems of the body *, including causing depression * *.
Depression itself is a common comorbidity in cancer * *, however, 6-42% of patients with cancer are already severely depressed at the time of diagnosis * *, which forces us to rethink the causal relationship between cancer incidence and the state of mind of a person. And during therapy, the prevalence of moderate-severe depression in patients reaches 76% *, which is many times higher than the average level of its prevalence in the population.
Reducing anxiety not only improves quality of life, but can also contribute to improved treatment outcomes. Chronic stress reduces sensitivity to leptin (the main regulator of energy balance) and alters the functioning of the dopamine system, which contributes to obesity. In addition, it markedly increases the levels of pro-inflammatory cytokines (IL-6) * and worsens the survival rate of patients.
Passion for work, hobbies, relaxation, relaxing activities, communication with friends, pleasant discoveries, positive emotions contribute to reducing stress levels. Walking in nature can reduce the level of the stress hormone cortisol by 15%, reduce heart rate and blood pressure by 4%, increase the number of immune cells (natural killer cells) in the blood by 50%, reduce glucose levels and mental stress *.
Some natural substances help to gently relieve internal tension without causing addiction when taken for a long time (about 6 months) *.
• Gamma-aminobutyric acid (GABA, pregabalin) gently relaxes and improves mood. Dosage: 3×0.5 g.
• Valerian (Valeriana officinalis). The root of the plant contains valerenic acid, which can enhance the effects of GABA in the brain. Daily dosage: 60 mg extract (1'000 mg dry root) of valerian.
• Melatonin (6 mg orally in the evening for 3 months) significantly reduces the risk of depression in breast cancer patients after breast surgery *.
• Vitamin C (1'000 mg) helps to reduce anxiety, presumably by slightly activating opioid-like receptors * and receptors for the neurotransmitter GABA *.
• Golden root (Rhodiola rosea). Taking 340 mg of Rhodiola extract in the morning and afternoon for 10 weeks reduces the anxiety of patients *.
• Ashwagandha (Withania somnifera) is another adaptogenic herb that reduces anxiety in patients (600mg/day extract for 12 weeks *).
• Water hyssop (Bacopa monnieri), aka Brahmi, suppresses inflammation in the brain *. Ethanol extract of the plant has been clinically shown to reduce feelings of anxiety * and improve cognitive performance * *. Dosage: 300-450 mg/day of extract, or 0.5 tsp (3 g) of plant powder for 3 months *.
• Anantavati, a herbal complex * containing the following sedative plants: Water hyssop (Bacopa monnieri), Asiatic pennywort (Centella asiаtica), Shankhpushpi (Convolvulus pluricaulis), Indian madder (Rubia cordifolia), Black oil plant (Celastrus paniculatus), Indian nard (Nardostachys jatamansi), Sway (Аcorus cаlamus). Dosage: 1 tab in the evening to improve sleep, and for anxiety conditions, an additional 1 tab in the afternoon. It is accepted no more than 1.5-2 months.
• Common fennel (Foeniculum vulgare) at normal dietary doses appears to be effective in postmenopausal women with depression and anxiety disorders *.
• Velvet bean (Mucuna Puriens), seed powder. Helps increase dopamine levels *. Dosage: 500 mg/kg.
• Herbal supplements containing Maypop extract (Passiflora incarnata): 3×0.5 g *; or benzoflavon 3×1 mg *; or a combination of L-lysine and L-arginine: 3 g/day * also suggest a positive effect in reducing anxiety.
• A systematic review of herbal remedies * highlighted as potential antidepressants for cancer patients such plants as Black cohosh (Actaea racemosa), Chamomile (Matricaria recutita), Vitex (Vitex agnus-castus), Lavender (Lavandula_angustifolia), Passionflower (Passiflora incarnata) and Saffron (Crocus sativus). Although their action is weaker compared to other plants considered, they are safer.
• Other natural supplements can also make a great addition to an anxiety reduction program. These are B vitamins and S-adenosyl-methionine (SAMe), which are involved in the synthesis of hormones and neurotransmitters; as well as magnesium, selenium, N-acetyl-cysteine, vitamin D, probiotics *.
Dietary changes could also help in the overall fight against depression. High blood levels of ω-6 fatty acids and linoleic acid have been shown to be significantly associated with more severe depressive symptoms among women who survived invasive breast cancer *.
Depression has also been associated with chronic systemic inflammation, which is discussed in «Anti-Inflammatory Therapy» †. While the current theory of depression considers it to be caused by a lack of serotonin, an alternative theory suggests that it is caused by an excess of cytokines mediated by inflammation. If this is the case, then a decrease in systemic inflammation should lead to a decrease in the depressive state.
In addition to being suspected of initiating cancer, depression not only poisons life, but also significantly increases the death rate *. In a meta-analysis, depression and anxiety were associated with an increased risk of cancer incidence (by 14%), cancer mortality (by 21%), and all-cause mortality in cancer patients (by 24%) *. In one study, depression worsened the five-year survival rate of cancer patients by a factor of 3.5 compared to those with no symptoms of depression *.
In contrast, peace of mind, meditation or prayer, yoga classes, optimism and confidence in success contribute to rapid changes in gene expression *, and positive changes in serum proteins, antibodies, improving the body's overall immune response. In metastatic breast cancer, treatment of depression during the first year prolongs the median survival time by 28.5 months compared to untreated patients *.
The problem of a depressive state is that it does not cause a desire to get rid of it, and therefore requires external intervention. Serious depression requires the help of a psychiatrist. The two main classes of drugs for depression in cancer are tricyclic antidepressants and selective serotonin reuptake inhibitors (SSRIs) * such as escitalopram (5-20 mg/day) *. It is always worth evaluating the balance of benefits and harms of a particular drug. For example, use of SSRi has been reported to be associated with a 27% increase in breast cancer mortality * *. The final choice of drug is made by a specialist, taking into account the side effects of drugs, such as a decrease in the effectiveness of essential drugs, increased nausea and vomiting, or a disorder in brain activity.
Some drugs used in psychiatry, regardless of their main therapeutic effects, have also shown antitumor activity in vitro.
• Dibenzazepine, an antidepressant, is effective against hormone-dependent (MCF-7) breast tumors *. *.
• Valproic acid, used in epilepsy, enhances the effects of paclitaxel *, prevents mammosphere formation, and induces the death of hormone-dependent breast cancer stem cells (MCF-7) *. Valproic acid is a derivative of valerenic acid that comes from the root of Valerian (Valeriana officinalis). Dosage: up to 2'000 mg/day *.
Recommendations provided by the Society for Integrative Oncology * also include having a life purpose, yoga, meditation, music therapy and stress management * *. The complex interactions between the endocrine, nervous, and immune systems suggest an important role for the patient's mental state in their recovery. It has been observed that those who practice transcedal meditation, compared with the general sample, have 55.4% fewer hospitalizations for benign and malignant tumors *.
Retrospective work by Kelly Turner, specifically dedicated to the issue of the so-called «spontaneous remissions», revealed several common factors that are characteristic of all patients who have defeated cancer *. Most of them are more psycho-emotional than chemical-biological:
- solid reasons to live on;
- psychological support of the social environment;
- liberation from negativity and increase in positive emotions;
- following not calculation, but feelings and intuition;
- a radical change in diet and control of one's health;
- the use of herbs and supplements;
- deep spiritual practice.
It is vitally important for the patient not to withdraw into himself, to lead an active social life, full of physical activity, positive emotions and enhanced brain activity – communication, enthusiasm, search, knowledge and entertainment. Loneliness and social isolation are associated with a 29% increased risk of coronary heart disease and a 32% increased risk of stroke *, and they are associated by about the same percentage with all-cause mortality *.
A living environment rich in physical, social, emotional environment and the possibility of self-realization, through the dopamine-leptin mechanism, suppresses the functioning of mitochondria in cancer cells, thereby causing a lack of energy and death of cancer cells through apoptosis *. The positive effect of an emotionally «enriched environment» is complex; it is not just about regulating hormones produced in the brain and lowering leptin levels, but involves the whole body. In mice inoculated with a mouse mammary tumor, «enriched environment» housing for 9 weeks markedly reduced tumor development, in part by reducing COX-2 and Ki-67 levels, and increasing caspase-3 levels *.
Social media can offer psychological and practical support to people going through difficult and dramatic cancer experiences. The Internet provides many online groups and communities for communication between patients, both those under treatment and those who have completed it. The exchange of experience and advice from patients who have overcome the disease can help ease the burden of treatment, find meaning in their lives and confidence in the success of treatment. For people who feel their unity with God, prayers, fellowship with brothers and sisters in faith, service to others and their calling can also help overcome stress, depression and depression. Faith really works miracles.
One has to seek the help of a psychotherapist. Others manage to cope with problems on their own, for example, by using meditation or «healing visualization», i.e. imagining how the body is cleared of cancer cells and tumors in general. Still others cannot get out of their painful state without external help. In any case, psychological problems can and should be solved. The human body is an integral system, and it is impossible to get rid of a physical illness, having a sick spirit.
Normalization of blood pressure. An increase in blood pressure over 115/75 mmHg begins to increase the risk of cardiovascular mortality * *. Moreover, the risk of cardiovascular disease doubles for every increase in systolic pressure for every 20 mmHg and for every 10 mmHg diastolic pressure from the threshold value of 115/75 mmHg *.
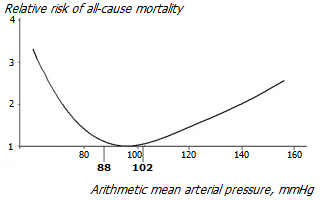
High blood pressure, meanwhile, may be a natural compensatory mechanism to increase blood flow to important organs such as the heart, kidneys, and brain *. This often happens when the function of the vascular system worsens. For example, with a loss of elasticity of blood vessels, or with a decrease in their internal section due to cholesterol deposits. Despite its important preventive benefit, lowering blood pressure has the potential to reduce blood flow with negative consequences. Thus, you should aim your treatment at eliminating the causes of high blood pressure, and not eliminating its consequences.
Aggressive drug treatment to lower blood pressure can cause side effects such as impaired cognition and kidney function * *. The latter can be controlled by such objective indicators as glomerular filtration rate (normal – 110 mL/min), creatinine and cystine-C levels. Therefore, it is better when the decrease in blood pressure occurs gently and smoothly, and is accompanied by measures to improve the blood supply to the organs.
Certain dietary and lifestyle changes can help lower blood pressure. This, in particular, regular physical activity * *; low-calorie diet * * high in fiber (30 g/day) and potassium (4.7 g/day) * and low in sodium *; alcohol restriction * and NSAIDs such as ibuprofen *.
In addition, some of the natural substances discussed below can help normalize blood pressure.
• Garlic (Allium sativum) lowers blood pressure in people with hypertension. Long-term use of aged garlic extract reduces systolic pressure by 5.1-16.3 mmHg and diastolic by 2.5-9.3 mmHg * * * by relaxing smooth muscle cells and dilating blood vessels without affecting blood pressure in people without hypertension. In addition, aged garlic lowers total and LDL cholesterol levels by 10% in patients with elevated cholesterol *. Dosage: 3.6 g/day of dry extract *.
• Melatonin relaxes the muscles in the blood vessels and suppresses the sympathetic nervous system, which together helps lower blood pressure *. Melatonin can lower nighttime blood pressure: systolic by 6 mmHg and diastolic by 3.5 mmHg *. Dosage: 3 mg/day at bedtime *.
• Grape seed proanthocyanidins reduce systolic blood pressure by 5.6% and diastolic blood pressure by 4.7% in pre-hypertensive individuals over 10 weeks *. Dosage: 300 mg/day *.
• Olive leaf extract (Olea europaea) for 12 weeks of admission is able to reduce systolic and diastolic blood pressure in individuals with stage 1 hypertension by an average of 11.5 mmHg and 4.8 mmHg respectively *. Dosage: 1'000 mg/day *.
• Celery seed extract (Celery) for 6 weeks in patients with mild to moderate hypertension can reduce systolic and diastolic blood pressure by 8.2 and 8.5 mmHg, respectively * due to vasodilating and relaxing effects. Dosage: 150 mg/day * of extract. Already 100 g per day of raw celery can show a noticeable effect.
• Quercetin lowers blood pressure through several mechanisms *, including through the blockade of angiotensin receptors. At the same time, its effectiveness is no worse than some pharmaceutical angiotensin blockers, such as irbesartan or losartan *. The magnitude of the reduction in blood pressure due to long-term use of quercetin can reach 5.7 mmHg *. Dosage: 150 mg/day * *.
• Stevioside, sweetener from Stevia (Stevia rebaudiana) acts as a calcium channel blocker, similar to verapamil. Stevizoid consumption throughout the year is able to reduce systolic pressure by about 4.5 mmHg *. Dosage: 750-1'500 mg/day *.
• Fish oils and ω-3 fatty acids improve cell membrane signaling and lower both systolic and diastolic blood pressure, and not just in hypertensive patients *. According to the results of a meta-analysis, taking omega-3 fatty acids (EPA+DHA) by hypertensive patients reduces systolic pressure by 4.5 mmHg, and diastolic pressure by 3 mmHg *. Dosage of fish oil: 2-4 g/day *.
• Coenzyme Q10 (CoQ10) has antihypertensive and cardioprotective effects. A meta-review shows that CoQ10 treatment leads to a slight decrease in blood pressure: systolic – by an average of 3.7 mmHg, and diastolic – by an average of 2 mmHg *.
• Magnesium is usually deficient in people with high blood pressure, and magnesium supplements can lower both their blood pressure. A meta-analysis shows that 400 mg of magnesium daily for 2 months can reduce systolic blood pressure by 2 mmHg and diastolic blood pressure by 1.5 mmHg *. Dosage: 500-1'000 mg/day.
• Other natural blood pressure correctors include resveratrol *, chlorogenic acid *, pomegranate extract (Punica granatum) * *, Hawthorn extract (Crataegus oxyacantha) *.
In fact, almost all of the listed funds are anti-inflammatory drugs; and you should expect the same healing effect from any other antioxidant and anti-inflammatory drugs.
Complete sleep. Poor quality sleep leads to an inadequacy of the immune system, which leads to the risk of not only cancer, but also any other diseases. Sleep disorders are observed in 30-50% of various groups of cancer patients * which is almost three times higher than the average level in the population *. Patients have insomnia and frequent awakenings at night and frequent short naps during the day, and sleep disorders only worsen during treatment *. Sleep efficiency is directly related to survival and may serve as a prognostic marker for patients with breast cancer *.
The following over-the-counter medications may be used intermittently to improve sleep quality.
• Valerian, plant root. Dosage: 60 mg extract at bedtime (equiv. 450-900 mg root *).
• Gamma-aminobutyric acid (GAMA), a mild neurotransmitter and psychostimulant. Dosage: 1'500 mg/day.
• Melatonin, sleep hormone. Sleep disturbances in patients with breast cancer are often associated with circadian rhythm disturbances and, accordingly, with a decrease in melatonin levels. Melatonin increases the levels of gamma-aminobutyric acid and serotin in the brain and hypothalamus. Those over 40 can take melatonin for a long time without first having their levels checked. Dosage: 3-6 mg strictly in the evening, 0.5-1 hour before bedtime.
• Food and drinks taken with dinner can significantly affect the time you fall asleep and the quality of your sleep. Eating a plant-based diet rich in polyphenols can help reduce your nighttime sleep *. Kiwi *, Cherry *, Soybean and Lima Bean * are recommended to improve falling asleep 1 hour before bedtime. Malted milk allows for deeper sleep *. At the same time, a low intake of complex carbohydrates, just like a high intake of fats or simple carbohydrates, can cause sleep disturbances *.
Diet in general has a profound effect on the quality of sleep. So, a small amount of animal protein and a large amount of complex carbohydrates in the diet contributes to the production of melatonin, while a large amount of protein acts excitingly on the nervous system, making it difficult to fall asleep *.
A calm transition to sleep can be helped by subdued red lighting, meditation, yoga, soft relaxing music.
Bedtime. The quality of sleep is directly related to the circadian rhythm. The time before midnight is considered the most favorable for the so-called phase «slow» sleep, during which growth hormone is produced. Therefore, it is often said that one hour of sleep before midnight is more valuable than two hours after midnight. Indeed, research shows that falling asleep between 10 pm and 11 pm is associated with a lower risk of heart disease than later or earlier times *.
The duration of a full sleep, as shown by a meta-analysis of studies, should be in the range of 7-8 hours.
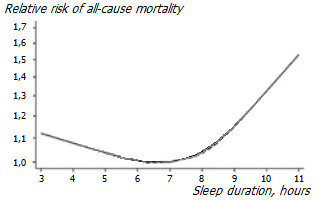
Reducing the duration of sleep can increase the risk of hormone-dependent breast tumors *, which may be associated with a decrease in the duration of action of melatonin. However, increased sleep duration is not a protective factor. Conversely, compared with 7–8 hours of sleep a night, more than 9 hours of sleep was associated with a 48% increased risk of breast cancer recurrence, a 52% increased risk of breast cancer death, and a 43% increased risk of all-cause death *.
Light mode. To comply with the circadian periodicity of light:darkness, sleep should be in the dark. Artificial lighting late at night destroys the light-sensitive nighttime hormone melatonin, which increases estrogen levels and, consequently, the risk of cancer. The absence of complete darkness during sleep, and even weak street light, negatively affect the level of melatonin, and with it the quality of sleep.
The blue part of the spectrum reduces melatonin levels more than others, and the red part less. Reducing artificial light, using glasses with amber lenses in the evening, and using smartphone apps that reduce blue light can alleviate circadian rhythm disturbances to some extent and reduce the risk of breast cancer *.
Clinical studies show that exposure to light can affect body fat formation * * as well as the appetite-regulating hormones leptin and ghrelin *. Shorter sleep duration, as well as late sleep, has been associated with higher body mass indices * in numerous studies. Morning sunlight for at least 45 minutes (6 am to 9 am at 1'300 lux) for 3 weeks resulted in a decrease in fat mass and appetite in obese women *. Moreover, such an effect of light was not associated with a change in the calorie content of the diet and the duration of sleep *. Thus, early awakening contributes to weight loss.
Chronic lack of sleep is associated with disruption of thyroid hormones *. In addition, lack of sleep increases blood sugar levels and the stress hormone cortisol, which reduces androgen levels and increases the imbalance between estrogen and androgen. Since hormones work like a team, disruption of the natural circadian cycle negatively affects hormonal balance and overall health.
Temperature regime. The night temperature in the bedroom should be lowered, following the natural diurnal temperature fluctuation.
Latent infections are not just a threat of exacerbation of inflammation and loss of internal resources. Infections are largely responsible for the appearance of cancer, and getting rid of latent infections can greatly strengthen the patient's position against his disease. If the infectious cause of cancer is not eliminated, or at least the infection is not made passive, the disease will inevitably return again and again.
Viruses. Herpes virus, Epstein-Barr virus *, human papillomavirus, human polyomavirus are found in the vast majority of the population. Maintaining an adequate state of the immune system allows you to restrain their onset. Many herbal remedies known as antimicrobials and antifungals are also effective against various types of viruses *. For example:
- Licorice (Glycyrrhiza uralensis), root;
- Baikal skullcap (Scutellaria baicalensis), root;
- Salvia (Salvia officinalis), leaves;
- Self-heal (Prunella vulgaris), leaves;
- Black elderberry (Sambucus nigra), fruits;
- Eleuthero (Eleutherococcus senticosus), root;
- Hyssop (Hyssopus officinalis), leaves;
- Milk thistle (Silybum marianum), seeds;
- Garlic (Allium sativum), root;
- Ginseng (Panax ginseng), root;
- Turmeric (Curcuma longa), root;
- Lemon balm (Melissa officinalis), leaves;
- Pomegranate (Punica granatum), fruits and pericarp.
Fungi. Most often, it is Candida (Candida), fungi that are present on the mucous membranes of almost every adult *. About two dozen species of candida are known; however, the vast majority of infections are caused by Candida albicans, Candida glabrata, Candida parapsilosis, Candida tropicalis, Candida auris and Candida krusei *.
Candida infections are common in hospitalized patients and in the elderly. The difficulty of completely eradicating candida is due to its ability to switch between yeast and filamentous forms of existence, as well as its ability to form biofilms that offer serious resistance to chemotherapy. The widespread use of antifungal drugs has given rise in recent years to drug-resistant forms of candida.
Although it is unlikely that fungi can be permanently eliminated, it is possible to contain them with some natural remedies without resorting to synthetic antifungal drugs.
- Essential oils of Pogostemon (Pogostemon heyneanus) and Indian bay leaf (Cinnamomum tamala) leaves effectively destroy the protective polysaccharide biofilm of Candida in vitro *.
- Essential oils of other plants have also shown significant antifungal activity in vitro, e.g. Dill (Anethum graveolens) seed oil * *, Cilantro (Coriandrum sativum) seed oil, Ginger (Zingiber officinale) herb, Peppermint (Mentha balsamea) herb, Lemongrass (Cymbopogon) herb, leaves of Eucalyptus (Eucalyptus), Cinnamon (Cinnamomum zeylanicum) (listed in ascending order of effectiveness) *.
The essential oil of cinnamon causes the destruction of the cell wall and candida organelles. The complex of cinnamon oil and pogostemon oil showed strong antifungal activity against Candida albicans, Candida tropicalis and Candida krusei. In patients who took 54 mg of cinnamon oil and 27 mg of pogostemon oil three times for 14 days, the cure rate of intestinal fungal infection was 72%, and the improvement rate was 28% *.
Bacteria. Overdose of niacin (vitamin B3) in the event of an infection can greatly increase the ability of the innate immune system to fight against staph infections, including those resistant to antibiotics *.
The elimination of latent infections not only reduces the level of general inflammation, but also eliminates the constant source of infections. An example can be dead teeth and their remains – a place difficult for immune cells to reach, where various microorganisms can hide and wait for the moment when the body's resistance weakens.
Many plants used as spices show a pronounced antibacterial and antifungal effect:
- Clove (Eugenia caryophyllata), flower buds;
- Garlic (Allium sativum), bulbs;
- Oregano (Origanum vulgare), flowering stem tops;
- Thyme (Thymus vulgaris), aerial part;
- Cinnamon (Cinnamomum zeylanicum), tree bark;
- Cumin (Carum Carvi), seeds;
- Cilantro (Coriandrum sativum), seeds;
- Rosemary (Rosmarinus officinalis), leaves;
- Ginger (Zingiber officinale), root;
- Basil (Ocimum basilicum), aerial part;
- Fennel (Foeniculum vulgare), seeds;
- Black pepper (Piper nigrum), grains; and others *.
All of them suppress the development of pathogenic bacteria, and can be beneficial for intestinal health.
Oregano oil, garlic cloves, myrrh and thyme leaves, cinnamon bark, black pepper seeds, cumin seeds show strong in vitro activity against some «drug-resistant» forms of bacteria that most antibiotics do not kill. Cat's claw (Uncaria tomentosa) extract, grapefruit seed extract, artemisinin, oils of oregano, cinnamon, clove bud, citronella, and wintergreen were effective in vitro against Lyme bacteria.
A mixture of these spices, added to food, could presumably have a noticeable positive effect.
Antiparasitic activities. A significant part of the adult population, without even suspecting it, are carriers of one or more types of parasites. Foreign agents are responsible for about 20% of all cancers *, and the pattern of infection by intracellular parasites and the pattern of oncogenesis are very similar in terms of metabolic disturbances *, cell signaling and control of gene expression * *. Because of this, the mechanisms that act against cancer cells can also work against many parasites, and vice versa, antiparasitic agents can destroy both at the same time *.
The vast majority of common parasites colonize mainly the large intestine, but some of them are able to infect other parts of the body.
Identification of a particular parasite allows you to choose the best method of dealing with it. In addition to specialized remedies, some natural remedies are used to combat intestinal parasites. The following are the best clinically studied, and if necessary and in consultation with the doctor, the following natural antiparasitic agents can be used.
• Neem, aka Margosa (Azadirachta indica), leaf extract or essential oil. The plant is effective against protozoa, fungi, microbes and viruses. Because of the bitter taste, the extract is best taken as a capsule: 2×250mg for up to 1 month. Courses should not be frequent; but only when absolutely necessary. It is worth remembering that neem extract greatly reduces the secretion of gastric acid; and besides, it is a strong contraceptive that affects the maturation of the follicles.
• Artemisinin, extracted with dichloromethane or ethanol (but not water!) from Sweet wormwood (Artemisia annua), is a broad spectrum antiparasitic originally used for malaria. Artemisia is active against a wide range of parasites, bacteria and even some viruses. Artemisinin and other artemisin substances are taken in capsules, 6×500 mg * for 15 days. The course is repeated as needed. Artemisin substances create high oxidative stress inside the cells; therefore, to increase their effectiveness for the duration of artemisinin therapy, all antioxidant supplements are canceled.
• In folk medicine, the following plants are also used as antiparasitic agents:
- Feverfew (Tanacetum parthenium), flowers;
- Wormwood (Artemisia absinthium), aerial part;
- Clove (Syzygium aromaticum), flower buds;
- Black cumin (Nigella sativa), seeds;
- Nutmeg (Myristica fragrans);
- Black walnut (Juglans nigra), leaves, green peel and internal partitions;
- Eucalyptus (Eucalyptus), leaves;
- Ginger (Zingiber), root powder;
- Kamala (Mallotus philippensis), kamala;
- Garlic (Allium sativum), bulb; and others †.
They are taken both orally and in the form of enemas – 1-2 times a year for at least 30 days – as needed or prophylactically. However, they are all less effective than specialized antiparasitic agents.
Intracellular parasites are of particular concern because of their ability to induce an indolent chronic inflammatory condition, promote malignancy, and tolerate antibiotic treatment.
To date, at least 10 species of mycoplasmas alone have been found against the background of at least 15 types of cancer affecting the brain, mammary gland, lymphatic system, various organs of the genitourinary, respiratory, gastrointestinal and urinary systems *. Once inside the body with a tick bite, mycoplasmas can conduct their covert sabotage activities for many years, significantly increasing the risk of cancer.
The actual incidence of diseases spread through insect bites may be two to three orders of magnitude higher than official data. The problem is that they are difficult to recognize, and doctors are not taught to pay attention to them. It is hard to imagine how many people suffer from them, but because of the wrong diagnosis, they are unsuccessfully treated for other diseases.
To get rid of such intracellular parasites as Borrelia, Anaplasma, Babesia, Ehrlichia, Bartonella, the following natural complex is recommended as a base:
- Sage (Salvia miltiorrhiza), root; to reduce inflammation and support spleen function;
- Baikal skullcap (Scutellaria baicalensis), root; to reduce inflammation;
- Sweet wormwood (Artemisia annua), leaves; for direct destruction of parasites;
- Milk thistle (Silybum marianum), seed; to support liver function;
- Mongolian milkvetch (Astragalus membranaceus), root; to protect the bone marrow;
- L-arginine to improve endothelial function;
- Ashwagandha (Withania somnifera), root; to reduce inflammation;
- Licorice (Glycyrrhiza glabra), root; for immunomodulation;
- Magnolia berry (Schisandra chinensis), fruits; for immunomodulation.
Unfortunately, it may take many months and even years of systematic and persistent struggle, and a long individual selection of the composition of the plant complex, to get rid of such infections. A good guide for people who have fallen prey to such parasites is the books by Stephen Harrod Buhner.
Detoxification and organ support. Detoxification is the process of removing useless and harmful agents from the body – from chemical elements to foreign organisms. A healthy body in adequate conditions of existence naturally removes toxins of both internal origin and (to a certain level) toxins that have entered it from the outside. However, these conditions are not always met. In addition, the problem of exogenous toxins is growing every year. Their number multiplies, diversity increases, and their combination can act synergistically. And no matter how hard we try to avoid things and food containing toxins, it is impossible to do this completely.
Some toxins can quickly bind and be excreted. However, staying up to this point inside the body, they exert their carcinogenic effect *. Other toxins, such as heavy metals or persistent organic pollutants *, are much more difficult to eliminate. They accumulate in various tissues, especially in fat-containing * such as the mammary gland, and can even be transmitted to infants through breastfeeding *.
Toxins are one of the most important causes of inflammation and cancer. Getting rid of them could reduce the risk of cancer in healthy people and create the necessary basis for the recovery of patients. Naturopaths, even relatively healthy people, suggest detoxification activities at least once a year. The detoxification procedure is especially important for cancer patients during antitumor therapy, when the body is filled with a large amount of decay products of dead cells and needs to be removed.
Official medicine is skeptical about the possible problems of chronic low-level accumulation of certain toxins, does not conduct research in this area, and is limited to detoxification only in case of acute poisoning. It is believed that the organs are able to effectively cope with the removal of a variety of toxins, and a low pollution background is not dangerous. Therefore, there are no clinical guidelines for general body detoxification, and all recommendations in this area come from alternative sources. All of them are not clinically proven, and have the status of assumptions. However, they will be considered because they work not only for detoxification, but also for supporting the work of various organs.
The body has four main ways of removing toxins – breath, sweat, urine and feces. The more elimination pathways involved, and the more detoxifiers involved, the deeper the cleansing process goes, and the longer the list of toxins removed. The sequence of detoxification suggested by naturopaths is as follows: skin and intestines → kidneys and lungs → liver and gallbladder → lymphatic and circulatory systems. That is, in the reverse order of how toxins move from the body to the exit.
Skin. The removal of toxins through the skin occurs mainly through the pores of the sweat glands. The first priority should be to keep the skin clean so that the toxins that are thrown out are not absorbed back. Sauna (Finnish or infrared) can be a powerful tool for detoxifying the body through the skin *. Although the high temperature kills cancer cells and is therefore used for hyperthermia, the sauna can cause swelling of the hands after axillary surgery *. There is also an understandable concern that increased fluid circulation in the body without the simultaneous use of cytotoxic agents may promote metastasis. However, if you follow this logic, then it would not be worth recommending physical activity, which in the same way accelerates the lymph.
Intestines. Vegetable food, rich in fiber, provides regular stools and a fairly high-quality bowel cleansing. In contrast, foods rich in gluten, meat, and solid fats contribute to poor intestinal mass movement and an unfavorable bacterial spectrum. Therefore, for vegetarians, the problem of bowel cleansing is unlikely to be relevant, unlike lovers of delicacies.
Enriching the diet with vegetable fiber will be enough to cleanse the intestines and keep it in proper tone. Fiber shortens the transit time of the food mass, binds toxins and carcinogens, and feeds beneficial intestinal microflora *. Fiber has two forms – soluble and insoluble. Soluble fiber is found in fruits, berries, oat bran, legumes, and apple pectin. Insoluble fiber is found in vegetables and whole grains, such as wheat bran. The therapeutic dose of fiber is at least 35 g/day. Recall that when consuming fiber in the form of a supplement, it is necessary to consume an adequate amount of water.
Of the additional funds, if necessary, the following two compositions can be used within 2-3 weeks.
• Intestinal stimulant composition: Buckthorn (Frangula alnus), bark; Aloe (Aloe ferox), leaves; Senna (Cassia officinalis), leaf and bean; Cascara (Rhamnus purshiana), bark; Barberry (Berberis vulgaris), root bark; Ginger (Zingiber officinale), rhizome; Garlic (Allium sativum), bulb; Cayenne pepper (Capsicum annuum), fruit; castor oil. Such a mixture slows down absorption, which leads to a thinning of the intestinal mass, and also irritates the intestines, which leads to its more active release. With irritated intestines, this composition is used with great care.
• Enveloping and adsorbing composition: Broadleaf plantain (Plantago major), seed; Flax (Linum usitatissimum), seed; Slippery elm (Ulmus rubra), inner bark; Marshmallow (Althaea officinalis), root; Fennel (Foeniculum vulgare), seed; apple pectin. Swelling, they form a jelly-like mass that cleanses the walls and pockets of the intestines, absorbs toxins and stimulates the intestines.
For the same purpose, you can use bentonite clay, approved for use inside. As an adsorbent, clay may be a better choice than activated carbon. By absorbing and retaining toxic substances, adsorbents do not allow them to be reabsorbed into the bloodstream, and allow them to leave the body along with feces. However, it is worth remembering that adsorbents do not act selectively, and can interfere with the absorption of substances needed by the body in the intestines.
A clear indicator of the normalization of the digestive tract is the regularity (1-2 times a day) and the consistency of the stool. The remains of a normally assimilated and formed food mass should look like a snake; come out quickly, completely, and without leaving a sticky residue.
Lungs. The epithelium of the lungs can be contaminated due to smoking, occupational factors or other causes of air pollution. Although the lungs have a natural ability to clear out toxins that enter them, these mechanisms are not always successful in dealing with chronic challenges such as tobacco tar.
Unfortunately, we do not have the ability to mechanically clear the surface of the lungs, as can be done with the intestines. And many contaminants, such as asbestos or silicates, ingrained in living tissue, are unlikely to be removed at all. However, to some extent, we can reduce the toxic load on the lungs and help them eliminate other accumulated toxins and carcinogens.
First of all, the possibility of air pollution – tobacco smoke, dust and other pollutants – should be avoided, and measures should be taken to purify and improve it – install an air purifier, an ionizer and an evaporator of volatile oils in the room.
The air purifier allows you to reduce the concentration of allergenic dust in the air, reducing the inflammatory state of the epithelium.
The air ionizer saturates the air with negative ions. The inhalation of ionized air, as well as the intake of any antioxidants inside, contribute to the restoration of lung epithelial cells damaged by toxins and counteracts the accumulation of microbes, fluid and sputum in the lungs and respiratory tract *.
Volatile oils evaporated indoors help improve epithelial health and restore lung function. To do this, you can take oils of eucalyptus *, fir *, oregano *, tea tree *, peppermint * and some others *.
Light jogging provides us with both deep saturation of the lungs with oxygen and a gentle vibration that helps to expel accumulated mucus. And reducing the consumption of meat and dairy products reduces the formation of mucus in the body. Proteolytic enzymes, such as serrapeptase, are able to break down mucus that clogs the airways, resulting in a decrease in its viscosity (stickiness and gel-like consistency). Because of this, they are useful for maintaining the cleanliness of the respiratory tract, especially in their chronic diseases.
The procedure for cleansing the lungs is a long process that may require more than one week, or even more than one month.
Kidneys. The kidneys directly remove liver-bound toxins from the body. They can be clogged with stones of different sizes and different chemical composition, but getting rid of them depends largely on the acid-mineral composition of the food and the level of general inflammation.
In herbal medicine, the following herbal remedies are used to support and manage kidney function.
• Cranberry juice (120-300 ml/day) suppresses urinary tract infections * *.
• Goldenrod (Solidago virgaurea), grass; tones the urinary tract and aids in kidney detoxification *.
• Bearberry (Arctostaphylos uva-ursi), leaves; acts as a diuretic and a natural antibiotic that is excreted through the urinary tract.
• Marshmallow (Althaea officinalis), leaves and root; and Chamomile (Matricaria recutita), flowers; act as an anti-inflammatory and antispasmodic agent.
• Burdock (Arctium minus), root; and Barberry (Berberries vulgaris), root; act anti-infectious in the urinary system.
• Dandelion (Taraxacum officinalis), leaves and root; Juniper (Juniperus communis), leaves and berries; Horsetail (Equisetum arvense), stem; Plantain (Plantago lanceolata), leaves; act as a diuretic, helping clear infection and prevent the growth of kidney stones *.
• Iodine in the form of Lugol's solution (2 drops per day) helps reduce the acidity of urine *.
The pancreas produces digestive and metabolic enzymes, as well as a hormone such as insulin.
• Gymnema (Gymnema sylvestre), leaves; supports the pancreas and restores its damaged cells. Ethanol extract of gymnema increases the number of islets and beta cells in artificially induced diabetes in rats * *. Human equivalent dosage: 300 mg/day of extract *.
• Melatonin stimulates the secretion of pancreatic enzymes *. In addition, melatonin is a powerful antioxidant that reduces damage to the pancreas and protects tissues from inflammation *.
• Other antioxidants, such as curcumin from turmeric root (equiv. 1'200 mg/day) *, or proanthocyanidins from grape seeds (equiv. 1'200 mg/day) *, also reduce the toxic effects of oxidants by protecting pancreatic tissue by attenuation of inflammatory reactions.
The liver is the central organ that binds a wide variety of toxins and prepares them for removal, including xenoestrogens and dangerous estrogen metabolites. At the same time, the liver does not accumulate metabolic products in itself, therefore it does not require any special cleaning. But if the liver is bad at binding toxins, and the kidneys are bad at removing them, the toxic load on the body grows, and the liver can be damaged by various chemicals, in particular, chemotherapy drugs.
Hepatoprotectors support liver function and show antitumor properties.
• Broccoli (Broccoli), and somewhat worse kohlrabi, cauliflower, and other cruciferous vegetables, activate phase II detoxifying enzymes; in particular, glutathione-S-transferase (GST) * * *. It is helpful to know that 3-day-old sprouts of many cruciferous varieties, including broccoli and cauliflower, contain 10-100 times higher levels of their active ingredient, glucoraphanin, than their mature plants *. Thus, a small amount of broccoli sprouts can be just as effective in protecting against cancer as much larger amounts of an already grown vegetable.
Again, as in the case of vitamins, we are talking about the restoration of physiological levels of glutathione, and not about its excess. In patients undergoing chemotherapy, GST can detoxify chemotherapy drugs, thereby increasing tumor drug resistance.
• Milk thistle (Silybum marianum), finely ground seeds. Due to the presence of silymarin, milk thistle reduces liver damage from radiation and chemical damage, including chemotherapy *. Silymarin dosage: 3×140 mg orally for several months *.
• Good-King-Henry (Blitum bonus-henricus). The methyl extract of the root in animal experiments shows a hepatoprotective effect that is twice as weak compared to silymarin (equiv. 2'400 mg/day of dry extract) *.
• Licorice (Glycyrrhiza glabra), root. The main active ingredient in licorice is glycyrrhizin, a conjugate of glucuronic acid and glycyrrhetinic acid. Dosage of glycyrrhizin: 200-600 mg/day, which corresponds to approximately 5-15 g/day of dry root *.
• Turmeric (Curcuma longa), finely ground root. Curcumin dosage: 1 g/day *, which corresponds to approximately 50 g (8 tbsp) per day of turmeric powder. Turmeric also helps to avoid stagnation of bile in the gallbladder *.
• Dandelion (Taraxacum officinale), finely ground root. Dry root dosage: 1.5-24 g/day *. An ethanol extract of the root (equiv. 5'000 mg/day po) markedly reduced liver damage caused by the chemical carcinogen in animal studies * *.
• Artichoke (Cynara scolymus). Artichoke leaf extract is commonly found in liver detox supplements. Taking artichoke extract (600-1'200 mg/day for 2-3 months) helps to slightly lower cholesterol levels in patients *, increase blood flow through the liver, and also reduce total bilirubin *. However, in chronic hepatitis C, even 3'200 mg/day provided only symptomatic improvement *.
• Agrimony (Agrimonia eupatoria), aerial part. Promotes a better outflow of bile from the liver and gallbladder, reducing the risk of stone formation. Take 1-2 glasses per day in the form of an aqueous infusion, for which 1 tbsp. herbs are poured with 1 cup of boiling water, boiled for 2-3 minutes, and insisted for another 10 minutes.
• Betaine, sometimes referred to as vitamin B16, enhances the ability of tissues to take up oxygen and help detoxify waste products to support the liver. Dosage: 1'000 mg/day.
• Calcium D-Glucarate assists the liver in detoxifying and removing excess estrogen and «bad» estrogen metabolites.
• Other well-known liver protectors *:
- Baikal skullcap (Scutellaria baicalensis), roots and rhizomes;
- Black cumin (Nigella sativa), seed;
- Gotu kola (Centella asiatica), leaves;
- Boswellia (Boswellia serrata), resin;
- Burdock (Arctium lappa), roots;
- Garlic (Allium sativum), root cloves;
- Barberry (Berberis vulgaris), leaves, root bark;
- Hydrangea (Hydrangea arborescens), root;
- Oregano (Origanum vulgare), aerial part;
- Chicory (Cichorium intybus), root;
- lipoic acid.
The Institute for Functional Medicine has developed a specialized diet * that includes foods with nutrients that enhance the effectiveness of liver detoxification – mainly non-starchy vegetables, fruits and whole grains. This diet takes into account that different foods participate differently in both phases of detoxification, which allows them to be combined in the best possible way *.
Foods that are believed to help restore liver function: fish from polar waters containing taurine, polyunsaturated fatty acids, as well as ω-3, which ensure the normal functioning of the liver * *; carrots, controlling the secretion of bile acids *; beets *, garlic *, onions *, cauliflower and Brussels sprouts *, asparagus *, avocados *, green tea *, blueberries * that protect the liver from damage; broccoli *, walnuts *; olive oil, which reduces the accumulation of triglycerides in the liver *.
To protect the liver, it is equally important not only what we take, but also what we do not take. Avoid sugar and alcohol, and limit your fat and calorie intake as much as possible.
The lymphatic system is a kind of sewage system, purification and recycling of water in the body. It removes toxins from the intercellular space, and moves them to the filter stations (lymph nodes). Here, bacteria, viruses and toxins are absorbed and destroyed by lymphocytes and macrophages, after which the purified tissue fluid is returned to the bloodstream through the veins.
Sauna, along with massage, is a great way to increase the movement of blood and lymph, activate immunity and detoxification processes. However, despite a certain preventive effect, neither the first nor the second manipulation can be recommended for already diagnosed cancer until remission.
The movement of lymph is no less important than the movement of blood. But, unlike the circulatory system, the lymphatic system has neither a central nor a local pump that sets the lymph in motion. And the walls of the lymphatic vessels do not have a muscular frame. The movement of the lymph is provided solely by the movement of the surrounding tissue. The best manipulations to promote more active movement of lymphatic fluid are physical activity (especially jumping on a mini trampoline), yoga, massage, sauna and sufficient fluid intake.
Some natural remedies can improve the functioning of the lymphatic system * *.
• Cleavers (Galium aparine), Yellow bedstraw (Galium verum), aerial part, Figwort (Scrophularia nodosa), aerial part. Diosmin (modified hesperidin) derived from all these plants and its aglycone, diosmetin, protect the permeability of blood vessels, increase lymph flow and increase microcirculatory venous pressure, and in addition stimulate an increase in the number of thymic lymphocytes *. The percentage of lymphocytes proliferating under the influence of the ethyl extract of the bedstraw increases 7-8 times in vitro *. Ready-to-use forms of diosmin are available.
Daflon® (a combination of diosmin with hesperidin) improved lymph flow in dogs and rats *.
Linfadren® (a mixture containing diosmin, coumarin and arbutin) reduced swelling and improved hand function in patients after trauma or surgery *, including after breast surgery *.
• Aescin, contained in Horse chestnut (Aesculus) fruit extract, significantly increased lymphatic flow in dogs and reduced the formation of edema of various origins in rats (equiv. 4×1'000 mg) *.
• Calcium dobesilate (3×500 mg for 49 days) normalized lymph physiology and lymph flow rate in patients with chronic venous insufficiency *.
• Plant-based proteolytic enzymes (bromelain from pineapple, papain from papaya) help break down unwanted circulating proteins that promote swelling and inflammation *.
Some naturopaths also recommend plants such as White mistletoe (Viscum album), Knotted Figwort (Scrophularia nodosa), Golden saxifrage (Chrysosplenium), Red clover (Trifolium rubens), Buckbrush (Ceanothus cuneatus) to cleanse the lymph. In addition, Marigold (Calendula officinalis), flowers are considered plant lymphagons; Cilantro (Coriander sativum), plant greens; Burdock (Arctium lappa), root; Pokeweed (Phytolacca americana), root; however, no clinical evidence of their effectiveness has been found.
Cancer most often spreads by migration of cancer cells through the lymphatic system, and this process begins immediately after they appear. Therefore, it is extremely important not only to ensure the free movement of lymph flow, but also to ensure the effective functioning of immune cells. Increasing the removal of fluid from the tumor without an adequate response of immune cells can contribute to the spread of cancer cells *.
Some agents hostile to the body are, in principle, poorly excreted; and organs and systems can cope poorly with the removal of others. However, we have the opportunity to help the body get rid of them.
Chelation is the binding and removal of chemical toxins and heavy metals from the body. The aggressive chelation procedure is used for heavy metal poisoning, for which special substances are used *. Chelation, like any other medical procedure, should be carried out by specialists in a clinical setting, but not independently. Chelation procedures and specific tools are presented here for educational purposes only.
• Sodium alginate. Calcium alginate. Dosage: 3 g/day (6×500 mg), only 3-4 courses for 1-3 months.
• N-acetyl-cysteine (NAC). Dosage: 3'000-8'000 mg/day; taken for 6-12 weeks along with vitamin C (9'000-25'000 mg/day) in the form of potassium ascorbate.
However, it should be understood that metal chelation is not selective, and can remove not only arsenic, mercury and lead from the body, but also some useful metals such as zinc and magnesium, although much weaker. In addition, the chelation procedure can lead to other negative side effects.
Although enhanced chelation can be a useful point of recovery in some cases, it is not mandatory. More precisely, it is justified only with serious indications, for example, with laboratory-confirmed high levels of mercury or lead in the body. Chelating chemicals should not be used without a doctor's prescription. And during chemotherapy, aggressive chelation should be completely excluded.
At the same time, the consumption of chelating foods has no contraindications. Animal experiments show that cilantro has some chelating effect on mercury *, lead * *, cadmium *, and aluminum *; malic, citric and succinic acid – for aluminum *; chlorella – for lead *, mercury *, cadmium and zinc *; and citrus pectin – for lead *; and all of them seem to be useful in removing toxic metals in humans as well.
Halogens are easily replaced by other halogens, so bromine, chlorine or fluorine can be eliminated with iodine (12.5 mg/day) *. Women who daily took 12.5 mg of elemental iodine, the very next day, several times increased the degree of removal of mercury, lead and cadmium in the urine; and aluminum – not less than a month later *. However, if you use only food as a source of iodine, the detoxification process can take too long. The food dosage of iodine cannot be high, and iodine is the heaviest halogen, and therefore the least chemically active.
Progesterone and choleretic drugs are the most important factor in the removal of heavy metals. Our body has an innate detoxification system (using glutathione and methionine) that can be used in place of or in conjunction with chelators *. Metals are not present in the body in a free form, they are always associated with some kind of protein. With the help of certain enzymes, such as glutathione-S-transferase, they break away from the satellite protein and bind to glutathione, after which, with the help of ATP and magnesium, they are removed from the cell into the blood, enter the liver, and then pass into the intestine with bile and are removed from feces. Progesterone, like bitterness, promotes the outflow of bile and counteracts the reabsorption of heavy metals from the intestines into the blood.
It has been observed that in the presence of heavy metals (such as mercury or lead), antibiotics and antiviral drugs lose their effectiveness against certain infections. When patients with persistent relapses were treated for Chlamydia trachomatis infection or Herpes Simplex viruses, selective drug delivery along with administration of dried cilantro leaves (4×100 mg) or their methanolic extract helped to remove accumulated heavy metals from the body in the urine. As a result, traces of infections and clinical symptoms disappeared completely *.
It is likely that heavy metals impair the functioning of immune cells; and because there is often significant accumulation of mercury in cancerous tissues, chelation through food products may be of potential benefit. To do this, it is enough to add cilantro greens to food daily (5-10 g three times a day), carrot greens, asparagus, curly parsley, green tea, unsweetened apples.
In anecdotal reports, in patients with various types of cancer who used EPA (4×180 mg) and DHA (4×120 mg) as an antiviral agent, a dried cilantro tablet (3×100 mg) for heavy metal binding, and increased local delivery drugs to the affected area, there were marked improvements in cancer markers *.
Drinking mode. Since most of the toxins are eliminated with water, be sure to drink sufficient (but not excessive) amounts of fluid. Of course, you need to pay serious attention to its quality. It can be freshly squeezed juices, mineralized or electroactivated catholyte water (30 g per 1 kg of body weight). Adding lemon juice, lime juice or apple cider vinegar to the water enhances the detoxifying effects. Water used for cooking should be filtered.